You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
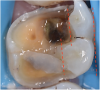
With all of the ongoing advancements in material science and technology, practicing dentistry is a dynamic and evolving process. Dental schools play a major role in shaping the way that dentistry is practiced. Educators have the responsibility of training future clinicians to able to deliver high quality dental care while producing restorations in an efficient and cost-effective manner, and instruction in the placement of partial-coverage restorations, such as onlays, is an important part of this training. Per The Glossary of Prosthodontic Terms published by the American Academy of Prosthodontics, an onlay is defined as a "restoration that restores one or more cusps and adjoining occlusal surfaces or the entire occlusal surface and is retained by mechanical or adhesive means"1 (Figure 1).
Partial-coverage restorations have been available as a treatment option in dentistry since the early 1900s. Historically, the material of choice for these restorations was cast gold.2 However, nowadays, the curricula of most dental schools in the United States and around the world no longer include teaching gold as a restorative material due to the significant increase in gold prices globally, the design complexity of the preparations required for such restorations, and the poor esthetics. During the past two decades, the use of all-ceramic restorations in dentistry has increased significantly, but the applications of contemporary ceramics have increased as well.3,4 Advancements in the mechanical and esthetic properties of contemporary ceramics have encouraged clinicians to use them in partial-coverage restorations (Figure 2).
Regarding the assessment of clinical outcomes of restorative procedures, it is of paramount importance for clinicians to realize that the longevity of the tooth is a more accurate metric than the longevity of the restoration. Conservative preparations protect teeth from the trauma caused by the excessive use of rotary instrumentation (Figure 3 and Figure 4).
Benefits of Partial-Coverage Restorations
When indicated, the benefits of placing a partial-coverage restoration instead of a full-coverage one are numerous, including the following:
· Preserving tooth vitality. A full-coverage crown preparation may result in an intrapulpal temperature increase of 16°F, which could lead to pulp necrosis due to the excessive heat generation.5,6
· Retaining tooth structure. The amount of tooth structure removed for partial-coverage preparations is approximately 34% to 39% compared with 74% for full-coverage restorations.7
· Reducing chairside time. With experience, the time that is needed to deliver a partial-coverage restoration is significantly less than the time needed for a full-coverage restoration.
· Facilitating impression making and cementation. For most partial-coverage restorations, retraction cord is not required, which eliminates or reduces the time spent on soft-tissue management before acquiring an impression (conventionally or digitally), and the cementation step involves less waste and enables easier cleanup of any excess cement.
· Increasing tooth longevity. Importantly, teeth that are restored with partial coverage restorations have lower endodontic complication rates when compared with those restored with full-coverage restorations.8,9
Guidelines for Partial-Coverage Preparations
To maximize the longevity of partial-coverage restorations, their preparations should be designed with simple geometry that includes all of the defective areas but does not involve any abrupt transitions (Figure 5). Proper reduction is key (Figure 6). Preparation designs for partial-coverage restorations are material dependent; therefore, the manufacturer's recommendations should always be followed. Generally, contemporary ceramics are required to be at least 1.0 mm to 1.5 mm thick when bonded using adhesive resin cements.
Regarding preparation design, the walls of preparations for partial-coverage restorations should be divergent to allow for path of insertion and have rounded angles to facilitate stress distribution (Figure 7). To develop a durable and long-lasting bond, the presence of enamel 360 degrees around the preparation's supragingival margin is essential (Figure 5). When assessing cuspal involvement, the preparation should include any cusp with a remaining thickness of less than 2 mm. This is critical to maintain the integrity of the tooth and, subsequently, the restoration (Figure 8).
Indicated Contemporary Ceramics
Although attempts have been made to use feldspathic porcelain and leucite-reinforced ceramics to fabricate partial coverage restorations,10 modern contemporary ceramics with enhanced physical properties are recommended, including the following:
· Lithium disilicate glass-ceramic. Whether it is pressed or machined, lithium disilicate (IPS e.max® CAD, Ivoclar Vivadent; Amber® Mill, Hass Bio America; Sagemax® Press, Sagemax) is the material of choice due to its excellent esthetics, strong mechanical properties, bonding ability, and proven track record of success.11,12
· Zirconia. Recently, zirconia (KATANA®, Kuraray; BruxZir®, Glidewell; IPS e.max® ZirCAD, Ivoclar Vivadent) is being used more often in partial-coverage restorations due to its outstanding mechanical properties and ability to be bonded using a specific bonding protocol.13 Due to the thickness of partial-coverage restorations, it is recommended to use the 3Y-TZP and 4Y-TZP zirconia, not the 5Y-TZP.14
· Hybrid ceramics. This is the newest category of materials to be used in partial-coverage restorations.15 Although these ceramics are not known for excellent mechanical properties and wear resistance, the resin content gives them a shock-absorbing property that enables them to function well clinically. Hybrid ceramics are either polymer-infiltrated ceramics or ceramic-infiltrated polymers (VITA ENAMIC®, VITA North America; CERASMART®, GC America; SHOFU Block HC, SHOFU, Inc.).
Conclusion
Partial-coverage restorations are great intermediate restorations that have the potential to prolong the life of any tooth; however, for long-term success, certain guidelines must be followed regarding their preparation design. Although the material of choice for partial-coverage restorations is lithium disilicate glass-ceramic, many other appropriate CAD/CAM materials have been introduced, such as zirconia and hybrid ceramics. There is a presently a lack of sufficient scientific literature supporting the use of these newer materials for partial-coverage restorations, but the early data shows promising results.
About the Author
Aous A. Abdulmajeed, DDS, PhD
Interim Director of Dental Materials
Associate Professor
Department of General Practice
School of Dentistry
Virginia Commonwealth University
Richmond, Virginia
References
1. The Academy of Prosthodontics; The Academy of Prosthodontics Foundation. The glossary of prosthodontic terms. 9th ed. J Prosthet Dent. 2017;117(5S):e1-e105.
2. Donovan T, Simonsen RJ, Guertin G, Tucker RV. Retrospective clinical evaluation of 1,314 cast gold restorations in service from 1 to 52 years. J Esthet Restor Dent. 2004;16(3):194-204.
3. Griffis E, Abd Alraheam I, Boushell L, et al. Tooth-cusp preservation with lithium disilicate onlay restorations: a fatigue resistance study. J Esthet Restor Dent. 2022;34(3):512-518.
4. Sulaiman TA, Abdulmajeed AA, Delgado A, Donovan TE. Fracture rate of 188695 lithium disilicate and zirconia ceramic restorations after up to 7.5 years of clinical service: a dental laboratory survey. J Prosthet Dent. 2020;123(6):807-810.
5. Zach L, Cohen G. Pulp response to externally applied heat. Oral Surg Oral Med Oral Pathol. 1965;19:515-530.
6. Valderhaug J, Jokstad A, Ambjørnsen E, Norheim PW. Assessment of the periapical and clinical status of crowned teeth over 25 years. J Dent. 1997;25(2):97-105.
7. Edelhoff D, Sorensen JA. Tooth structure removal associated with various preparation designs for anterior teeth. J Prosthet Dent. 2002;87(5):503-509.
8. Guess PC, Schultheis S, Wolkewitz M, et al. Influence of preparation design and ceramic thicknesses on fracture resistance and failure modes of premolar partial coverage restorations. J Prosthet Dent. 2013;110(4):264-273.
9. van Dijken JW, Hasselrot L. A prospective 15-year evaluation of extensive dentin-enamel-bonded pressed ceramic coverages. Dent Mater. 2010;26(9):929-939.
10. Abduo J, Sambrook RJ. Longevity of ceramic onlays: a systematic review. J Esthet Restor Dent. 2018;30(3):193-215.
11. Edelhoff D, Güth JF, Erdelt K, et al. Clinical performance of occlusal onlays made of lithium disilicate ceramic in patients with severe tooth wear up to 11 years. Dent Mater. 2019;35(9):1319-1330.
12. Malament KA, Margvelashvili-Malament M, Natto ZS, Thompson V, et al. Comparison of 16.9-year survival of pressed acid etched e.max lithium disilicate glass-ceramic complete and partial coverage restorations in posterior teeth: performance and outcomes as a function of tooth position, age, sex, and thickness of ceramic material. J Prosthet Dent. 2021;126(4):533-545.
13. Blatz MB, Alvarez M, Sawyer K, Brindis M. How to bond zirconia: the APC concept. Compend Contin Educ Dent. 2016;37(9):611-617; quiz 618.
14. Gupta S, Abdulmajeed A, Donovan T, et al. Monolithic zirconia partial coverage restorations: an in vitro mastication simulation study. J Prosthodont. 2021;30(1):76-82.
15. Lawson NC, Bansal R, Burgess JO. Wear, strength, modulus and hardness of CAD/CAM restorative materials. Dent Mater. 2016;32(11):e275-e283.