You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
Emergence Profile: The Need for Proper Planning
Dental implant treatment is an accepted treatment modality for successful tooth replacement.3 Long-term success of treatment depends on optimal implant position in addition to maintenance of soft-tissue health. The common occurrence of mucositis and peri-implantitis4 has demonstrated that soft-tissue health and thickness play important roles as a protective barrier to bacteria that can shorten the lifespan of dental implant treatment.5
Emergence profile can be defined as the contour of the tooth or restoration as it emerges from the gingiva.6 With dental implants, it is the contour of an implant restoration as it emerges from the implant platform. Placement of the implant platform in relation to the proximal contacts of adjacent teeth is critical to the development of ideal emergence profiles that will mimic the tooth being replaced. The emergence profile dictates the transformation of a dental implant into a natural-looking tooth. Successful maintenance of dental implants long-term requires adequate gingival thickness surrounding the implant; keratinized tissue of at least 1 mm to 2 mm is recommended.7,8 Thickness of the gingiva (mucosal thickness) also plays a factor in stability of the underlying hard tissue and bone stability crestally over time. When there is an initial tissue thickness of <2.5mm, bone loss of up to 1.45 mm can be expected over the first year of function.9-11Thicker tissue has demonstrated better long-term stability and resistance to implant-related disease than tissues of thinner biotypes.10
The diameter of the horizontal cross-section of the future crown at the gingival level will help determine the diameter size of the implant to be placed.12 The dimensions of the ridge in the buccal-lingual aspect will also influence the implant diameter selected.13 The distance between the crestal bone and the contact proximally with the adjacent teeth will have an influence on the appropriate implant depth to create an ideal emergence profile.14 Shorter distances between these two points will dictate a wider flare in emergence with a standard-diameter implant (4 mm) than when a wider implant is placed into the same space at the same depth.15 Longer distances between the points allow more gradual flare and are usually easier to manage than shorter distances.16
The depth of implant placement is dependent on whether the replacement is in the anterior or posterior zone.17 In the anterior zone typically the goal is to place the platform 3 mm to 4 mm below the cementoenamel junction (CEJ) of adjacent teeth.18 This allows for adequate room for emergence profile for esthetic purposes. In the posterior zone, the goal usually is to place the implant 2 mm to 3 mm below the CEJ of adjacent teeth.19 Depending on the type of implant system being used, the connection may allow for a deeper placement. Examples of such implant systems include Ankylos® (Dentsply Sirona, dentsplysirona.com), Bicon® (Bicon Dental Implants, bicon.com), and Neodent® (Straumann, straumann.com). Narrower-platform implant systems such as these that enable deeper placement allow for vertical room to compensate for the horizontal cross-section of the future implant crown.
It can be challenging to replicate not only the crown portion of the tooth but also the entire tooth anatomy. The cross-section of teeth at the gingival margin have various shapes, such as triangular, rhomboidal, and ovoid, depending on the type of tooth it is (Figure 1). The challenge arises because implants are round in cross-section at the platform and the clinician needs to transition to the specific shape of the natural tooth to provide natural-looking esthetics that mimic the profile of the tooth. Selecting the optimal implant diameter for the space available is dependent on not only the mesial-distal dimension but also the buccal-lingual dimension.20,21 Use of an implant with a narrower diameter than the mesial-distal space available may complicate emergence profile and lead to proximal food traps and adversely affect esthetics (Figure 2). This has clinical relevance in both the anterior and posterior areas of the mouth.
Tissue-level and non-platform-switched implants typically are not placed below the bone level (subcrestal) (Figure 3).22 Placement of such implants below the bone level is not recommended, as the bone will remodel leading to crestal bone loss in a saucerization pattern.11 This occurs in tissue-level implants because the smooth collar of the implant is not roughened for osseointegration. In non-platform-switched implants, subsequent placement of the abutment below bone level leads to remodeling circumferentially to accommodate biological width development (Figure 4).23
An optimal emergence profile helps to support the soft tissue around the implant restoration and prevents formation of food traps. Duplicating the emergence profile can be difficult, especially around multirooted teeth due to the horizontal cross-section size discrepancy at the CEJ level in comparison to a single implant.
The greatest challenges in developing ideal emergence profile are choosing an implant of a proper diameter and avoiding placing the implant in too shallow of a position.24 Placing an implant too shallow or in too narrow of a space, especially in the posterior zone, will likely lead to problems as there will not be enough running room for a laboratory to sculpt the tissue (Figure 5). Conversely, an implant placed with the platform 2 mm to 3 mm apical to the CEJ of the adjacent teeth will allow for the development of a more ideal emergence profile prosthetically (Figure 6).25 Running room is defined as the distance between the implant platform and the proximal contacts with the adjacent teeth.26 The apico-coronal positioning of the implant platform should adhere to the philosophy "as shallow as possible, as deep as necessary."27 This is, in essence, a compromise between esthetics and biologic principles.
A common misconception is that emergence profile can be controlled solely through the choice of implant diameter. In the posterior zone, a large horizontal cross-section is seen with molars. A wide-diameter implant will allow for ideal emergence profile, as it closely resembles the profile of the natural tooth at the CEJ level. A wide-diameter implant may be used assuming there is at least 2 mm of buccal and lingual thickness remaining after placement.28 Alternatively, a narrower implant may be chosen with subcrestal placement to allow for appropriate vertical room for emergence profile development. Clinicians should check with each dental implant manufacturer's recommendations and know the titanium grade to ensure that the implant can support the occlusal load of the site where the replacement is occurring.29,30 Patient parafunctional habits and bone density by zone of mouth also need to be critically examined to ensure long-term success without overload.31
Current methods to develop the soft-tissue emergence profile of dental implant restorations include the use of chairside custom healing abutments using incremental addition of resin or having a laboratory fabricate a custom healing abutment or temporary crown.32 After healing, the developed emergence profile is conveyed to the laboratory through the duplicated custom impression coping (Figure 7) or, alternatively, a digital scan of soft tissue using a scan body impression. This enables fabrication of a soft-tissue model that replicates the developed emergence profile intraorally. The laboratory can then create prosthetics that mimic the natural tooth emergence profile.
The following two case reports are examples of similar cases, one in which a traditional impression approach was used, and the other an intraoral scanner was utilized to capture the intraoral information.
Clinical Case 1
A 5 mm x 10 mm implant (MIS® V3, MIS Implants, mis-implants.com) had been placed at the mandibular first molar site and was ready for restoration. At the uncovering, a custom healing abutment that had been fabricated using an emergence profile management system (Cervico System™, VP Innovato Holdings Ltd, vpicervico.com) to match the emergence profile of a mandibular molar was inserted into the integrated implant, and the soft tissue was sutured around the abutment (Figure 8). After several weeks to allow the soft tissue to heal, the restoration phase began. The custom healing abutment was removed, revealing healthy soft tissue with an emergence cross-section that was relatively square, mimicking a molar (Figure 9).
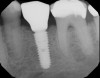
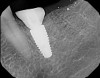
To avoid potential soft tissue collapse when the impression was captured, a custom impression abutment was created to support the soft tissue and properly communicate to the laboratory technician what had developed intraorally (Figure 10). This technique may be used with either open-tray or closed-tray impression abutments. The impression was taken and the custom healing abutment was reinserted intraorally while the laboratory constructed the restoration. The completed restoration was returned, the custom healing abutment was removed, and the implant restoration was inserted. The result was an emergence profile that mimicked a natural molar, enabling natural-looking esthetics (Figure 11). A radiograph demonstrated a smooth transition emanating from the implant platform to support an emergence profile that allowed soft-tissue maintenance and helped to eliminate potential food traps (Figure 12).
Clinical Case 2
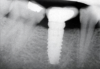
A 4.8 mm x 10 mm implant (Straumann® Bone Level Tapered [BLT], Straumann) had been placed at the mandibular first molar site and was ready for restoration. A custom healing abutment was fabricated and inserted at the time of surgical implant placement and soft tissue was sutured around the abutment using 4/0 Glycolon™ sutures (Osteogenics Biomedical, osteogenics.com) (Figure 13). A periapical x-ray was taken at the time of placement of the custom healing abutment to confirm full seating (Figure 14).
After a 6- to 8-week healing period, the custom healing abutment was removed to allow for a digital scan of the area as an alternative to conventional impression-taking (Figure 15 and Figure 16). An intraoral scan body was used to capture the soft-tissue profile and implant positioning with an intraoral scanner (CEREC® Omnicam, Dentsply Sirona) (Figure 17). Final seating of the restoration was performed with radiographic confirmation (Figure 18). The implant crown demonstrated a natural emergence profile to replace the mandibular first molar with optimized tissue fill in the interproximal regions (Figure 19).
Conclusion
Successful dental implant treatment as a modality of tooth replacement is measured not only by survival of the implant. Soft-tissue development is vital to the long-term success of dental implant treatment, in terms of both hygiene and healthy maintenance of the soft tissues surrounding the implant. Custom healing abutment design is an important aspect of effective lab communication and in achieving a predictable restoration.
Acknowledgment
The illustration portions of Figure 1 through Figure 3 were provided by Dr. Kurtzman. Figure 8 through Figure 12 are courtesy of Ioannis Vergoullis, DDS, MS.
Disclosure
The authors had no disclosures to report.
About the Authors
Mark Bishara, DDS
Private Practice, Bowmanville, Ontario, Canada
Gregori M. Kurtzman, DDS
Master, Academy of General Dentistry; Diplomate, International Congress of Oral Implantologists; Private Practice, Silver Spring, Maryland
Evan S. Krause, DDS
Fellow, International Congress of Oral Implantologists; Private Practice, Montville, New Jersey
References
1. Neale D, Chee WW. Development of implant soft tissue emergence profile. Implant Dent. 1995;4(1):62.
2. Steigmann M, Monje A, Chan HL, Wang HL. Emergence profile design based on implant position in the esthetic zone. Int J Periodontics Restorative Dent. 2014;34(4):559-563.
3. Raikar S, Talukdar P, Kumari S, et al. Factors affecting the survival rate of dental implants: a retrospective study. J Int Soc Prev Community Dent. 2017;7(6):351-355.
4. Roccuzzo M, Layton DM, Roccuzzo A, Heitz-Mayfield LJ. Clinical outcomes of peri-implantitis treatment and supportive care: a systematic review. Clin Oral Implant Res. 2018;29(suppl 16):331-350.
5. Valente NA, Andreana S. Peri-implant disease: what we know and what we need to know. J Periodontol Implant Sci. 2016;46(3):136-151.
6. Minoru S, Sato D, Baba K. Optimization of emergence profile of implant prosthesis: a literature review. Scientific Dental Journal. 2018;2(1):31.
7. Souza AB, Tormena M, Matarazzo F, Araújo MG. The influence of peri-implant keratinized mucosa on brushing discomfort and peri-implant tissue health. Clin Oral Implants Res. 2016;27(6):650-655.
8. Perussolo J, Souza AB, Matarazzo F, et al. Influence of the keratinized mucosa on the stability of peri-implant tissues and brushing discomfort: a 4-year follow-up study. Clin Oral Implants Res. 2018;29(12):1177-1185.
9. Linkevicius T, Apse P, Grybauskas S, Puisys A. The influence of soft tissue thickness on crestal bone changes around implants: a 1-year prospective controlled clinical trial. Int J Oral Maxillofac Implants. 2009;24(4):712-719.
10. Puisys A, Linkevicius T. The influence of mucosal tissue thickening on crestal bone stability around bone-level implants. A prospective controlled clinical trial. Clin Oral Implants Res. 2015;26(2):123-129.
11. Lombardi T, Berton F, Salgarello S, et al. Factors influencing early marginal bone loss around dental implants positioned subcrestally: a multicenter prospective clinical study. J Clin Med. 2019;8(8):1168.
12. Lazzara RJ. Criteria for implant selection: surgical and prosthetic considerations. Pract Periodontics Aesthet Dent. 1994;6(9):55-62.
13. Termeie D, Klokkevold PR, Caputo AA. Effect of implant diameter and ridge dimension on stress distribution in mandibular first molar sites-a photoelastic study. J Oral Implantol. 2015;41(5):e165-e173.
14. Tarnow DP, Cho SC, Wallace SS. The effect of inter-implant distance on the height of inter-implant bone crest. J Periodontol. 2000;71(4):546-549.
15. Siqueira S Jr, Pimentel SP, Alves RV, et al. Evaluation of the effects of buccal-palatal bone width on the incidence and height of the interproximal papilla between adjacent implants in esthetic areas. J Periodontol. 2013;84(2):170-175.
16. Gastaldo JF, Cury PR, Sendyk WR. Effect of the vertical and horizontal distances between adjacent implants and between a tooth and an implant on the incidence of interproximal papilla. J Periodontol. 2004;75(9):1242-1246.
17. Rismanchian M, Askari N, Shafiei S. The effect of placement depth of platform-switched implants on periimplant cortical bone stress. Implant Dent. 2013;22(2):165-169.
18. Berglundh T, Lindhe J. Dimension of the periimplant mucosa. Biologic width revisited. J Clin Periodontol. 1996;23(1):971-973.
19. Misch CE. Contemporary Implant Dentistry. 3rd ed. St Louis, MO: Mosby; 2010.
20. Belser UC, Bernard JP, Buser D. Implant-supported restorations in the anterior region: prosthetic considerations. Pract Periodontics Aesthet Dent. 1996;8(9):875-883.
21. Hermann JS, Buser D, Schenk RK, et al. Biological width around one- and two-piece titanium implants. Clin Oral Implants Res. 2001;12(6):559-571.
22. Saleh MHA, Ravidà A, Suárez-López Del Amo F, et al. The effect of implant-abutment junction position on crestal bone loss: a systematic review and meta-analysis. Clin Implant Dent Relat Res. 2018;20(4):617-633.
23. Pellicer-Chover H, Peñarrocha-Diago M, Peñarrocha-Oltra D, et al. Impact of crestal and subcrestal implant placement in peri-implant bone: a prospective comparative study. Med Oral Patol Oral Cir Bucal. 2016;21(1):e103-e110.
24. Saadoun AP, LeGall M, Touati B. Selection and ideal tridimensional implant position for soft tissue aesthetics. Pract Periodontics Aesthet Dent. 1999;11(9):1063-1072.
25. Tischler M. Dental implants in the esthetic zone. Considerations for form and function. N Y State Dent J. 2004;70(3):22-26.
26. Cavallaro Jr. JS, Greenstein G. Prosthodontic complications related to non-optimal dental implant placement. In: Froum SJ, ed. Dental Implant Complications: Etiology, Prevention, and Treatment. Oxford, UK: Wiley-Blackwell; 2010:157.
27. Buser D, William M, Belser UC. Optimizing esthetics for implant restorations in the anterior maxilla: anatomic and surgical considerations. Int J Oral Maxillofac Implants. 2004;19 suppl:43-61.
28. Merheb J, Quirynen M, Teughels W. Critical buccal bone dimensions along implants. Periodontol 2000. 2014;66(1):97-105.
29. Shemtov-Yona K, Rittel D, Levin L, Machtei EE. Effect of dental implant diameter on fatigue performance. Part I: mechanical behavior. Clin Implant Dent Relat Res. 2014;16(2):172-177.
30. Shemtov-Yona K, Rittel D, Machtei EE, Levin L. Effect of dental implant diameter on fatigue performance. Part II: failure analysis. Clin Implant Dent Relat Res. 2014;16(2):178-184.
31. Sheridan RA, Decker AM, Plonka AB, Wang HL. The role of occlusion in implant therapy: a comprehensive updated review. Implant Dent. 2016;25(6):829-838.
32. Wittneben JG, Buser D, Belser UC, Brägger U. Peri-implant soft tissue conditioning with provisional restorations in the esthetic zone: the dynamic compression technique. Int J Periodontics Restorative Dent. 2013;33(4):447-455.