You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
In dental laboratory technology, we have been designing and manufacturing removable partial dentures (RPDs) with conventional processes for more than 50 years. During the past few years, digital design capabilities have become a part of the RPD workflow. Whether the dental technician is using a conventional or digital workflow, he or she still needs to understand the basic fundamentals of RPD design. Goals in removable partial denture design are to restore function, enhance esthetics, and promote longevity. As M.M. DeVan, DDS, stated, our task is “the perpetual preservation of what remains rather than the meticulous restoration of what is missing.” It is with this thought that we study biomechanic design principles of removable partial dentures.
Removable partial dentures are defined as any prosthesis that replaces some teeth but not all in a partially edentulous arch and can be removed at will by the patient. Within this broad definition of partial dentures, one could include interim or provisional prostheses along with definitive removable prosthetics. A provisional or interim removable partial denture is a dental prosthesis used for a short time for reasons of esthetics, mastication, occlusal support, or for conditioning the patient to accept an artificial substitute for missing natural teeth until a more definite prosthetic dental treatment can be provided. Within this definition of provisional or interim prostheses, removable partials dentures such as stayplates, acrylic partials, and flexible-type partials are included. The emphasis of this article is on design and function of definitive RPDs that use a rigid framework for retention, support, and stability in the partially edentulous oral environment. Many concepts and philosophies in removable partial denture design are not possible to cover in this short article. The basic prosthodontic design concepts of a functional removable partial denture framework will be discussed.
RPD Diagnostics
All too often, dental laboratory technicians receive removable partial denture cases that have been planned improperly, which results in a DRPD (Drawer Removable Partial Denture). The patient who has paid for an RPD to restore compromised function or esthetics is unable to wear the unsuccessful appliance, so it is left in a drawer, and the patient increasingly does more dental damage to the remaining natural dentition.
This dental damage may include movement or super eruption of teeth, bone loss, decreased vertical dimension of occlusion, impaired phonetics, and loss of the confidence to smile or laugh. If our goal is to provide optimal removable prosthetic care and treatment for these dentally compromised patients, then a proper clinical and technical assessment of the oral condition is essential to a successful RPD.
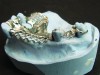
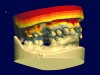
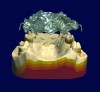
The RPD that successfully functions within a partially edentulous oral environment has been properly case planned with mounted diagnostic study casts.1 Clinical and technical evaluation of mounted study casts enables technicians to collect data to understand variables on the existing partially edentulous condition. These variables include condition of abutments such as clinical crown-to-root ratio, desirable and undesirable undercuts, rest preparation, inter-occlusal or inter-arch space, supporting tissues, and residual ridge anatomy (Figure 1 through Figure 3). Abutment, tooth, and occlusal modifications should be a routine part of clinical RPD protocols (Figure 4).
Figure 5 through 13 illustrate different situations and variables to consider during the diagnostic case planning process. When we spend more time on case planning, our success ratio on these complex prosthetic cases will increase. We must look at these removable prosthetic cases objectively to understand how future RPDs can be improved for the partially edentulous patient.
RPD Biomechanics
To understand the variables in RPD design or form, we must consider function first.
During function of an RPD, the prosthesis undergoes different types of stress. These stress forces during function include dislodging, horizontal, torsional, and vertical displacement forces. These displacement forces must be taken into consideration during the design analysis process.2 Creating resistance to this functional stress and displacement forces within our design is essential to the success of a definitive RPD. Resistance to functional stress and displacement forces is created through understanding 3 basic factors in RPD. design: retention, stability, and support. Retention is the resistance to vertical movement away from tissues and is provided by direct and indirect retainers. Stability is the resistance to lateral movement of an RPD and is provided by minor connectors, proximal plates, bracing clasp arms, and resin or metal denture bases. Support is the resistance to tissue movement (vertical or horizontal) of an RPD and is provided by rests, denture bases, and major connectors.
RPD Classifications
Kennedy’s method of classification is probably the most widely accepted system of classifying partially edentulous arches today. Although many of these arches are now having implants placed in the edentulous areas for fixed partial dentures, it is important to understand methods of classification for removable partials. Edward Kennedy, DDS, said that removable partials resting mainly on a compressible base over soft tissue must be so designed as to overcome excessive stresses of mastication and to prevent external forces on natural teeth or crowns that have attachments or now implants placed in them.
The Kennedy Classification System13 utilizes 4 classes of partially edentulous tooth loss:
Class I is a bilateral edentulous area located posterior to the remaining dentition. This class of RPD is the most common for partially edentulous patients. An example is when the first or second pre-molar plus molars are missing on both sides of the arch. Class I partials are tooth and tissue supported.
Class II is a unilateral edentulous area located posterior to the remaining dentition, such as when all the teeth are present on one side of the mouth and all are missing on the opposite side. The most common Class II is when a pre-molar and molars are missing on one side and present on the other side of the arch. Class II partial dentures are tooth and tissue supported.
Class III is a unilateral edentulous area with natural teeth located both anterior and posterior to it. This classification is most common when a second molar is present and the pre-molars plus second molar are missing. Implants and bridges are commonly used in these partially edentulous areas. Class III is a tooth-supported RPD.
Class IV is a single bilateral edentulous area located anterior to the remaining natural teeth. The most common Class IV removable partial is when the centrals and laterals are missing while all other teeth are present in the mouth. Class IV is a tooth-supported RPD.
RPD Components
The components of an RPD are major connectors, minor connectors, direct retainers or clasps, and indirect retainers.4 Various designs of major connectors may be used for RPDs, depending on the maxillae or mandible, edentulous areas, and anatomical arch form. The goal, as described by James S. Brudvik, DDS, is to “make every attempt to cover as little of the gingival tissues as possible.” Excessive gingival coverage is associated with increased plaque formation and should be avoided whenever possible.
Major Connectors
Major connectors on the maxillary arch should make every attempt to be 4-6 mm from the free gingival margins of remaining teeth. On the mandibular arch, major connectors should be 3-4 mm away from the gingival margins unless a lingual plate is indicated (Figure 14).
For a Class I Maxillary RPD, the most common major connector would be a posterior palatal coverage/plate (Figure 15). Although horseshoe major connectors are popular, they are less desirable biomechanically due to excessive flexibility. A horseshoe design for a major connector should be used in a Kennedy Class I to go around a palatal torus. A good rule is that more anterior tooth loss creating a larger posterior edentulous areas means more palatal coverage in major connector design.
With mandibular Kennedy Class I removable partial dentures, the most common is a lingual plate or lingual bar. When adequate lingual depth of at least 10 mm is present or an RPI or RPA clasp design is utilized, then a lingual bar is used as major connector.
If inadequate lingual depth is present, a high frenum attachment exists, or where residual ridges have excessive vertical resorption, then a lingual plate is chosen.
For a Class II Maxillary RPD, the most common major connector is a wide palatal strap that connects the posterior edentulous sides together. This type of palatal coverage is important to provide support and stability to the RPD. Horseshoe designs are commonly used as well, although they do not provide the support needed for a bilateral distal extension base RPD.
For a Class II Mandibular RPD, the most common major connector design is a lingual bar that has cross-arch stabilization to the dentate side of arch. If future anterior tooth loss is expected, or high lingual frenum attachment or inadequate lingual depth exists, then a lingual plate would be indicated.
For a Class III Maxillary RPD, the most common major connector is a single palatal strap that connects the edentulous area of the arch with the distal abutment to the dentate side. Horseshoe major connectors are used although not desirable due to flexibility and increased anterior palatal coverage.
For a Mandibular Class III RPD, the major connector of choice is a lingual bar with lingual plating reserved for inadequate lingual depth, high frenum attachment, or future anterior tooth loss.
For a Class IV Maxillary RPD, the most common major connector is a horseshoe design. The Class IV is largely tooth supported and commonly utilizes a rotational path of insertion RPD design. For a Class IV Mandibular RPD the most common is a lingual plate with a modified lingual bar extending to pre-molar or molar for clasping. Class IV RPDs have other challenges that include esthetics and function when incising food during mastication (Figure 16).
Direct Retainers/Clasps
The direct or clasp retainers can be distinguished between tooth-supported (Class III and IV) and tooth-tissue-supported (Class I and II) RPDs. With a Class I and II tooth-tissue-supported RPD design, the retainer clasp should provide stress breaking from the distal abutment. The distal abutment clasp would ideally have a self-releasing design for disengagement from the tooth during vertical movement under function. Such clasps include bar designs such as RPI, RPA, roach, or modified roach. Circumferential clasps such as round wrought wire with PGP (platinum-gold-palladium) or CrCo (chromium cobalt) provide retention and self-releasing during function and are an excellent option for distal extension bases. Distal abutments that have a high height of contour that cannot be modified are a good choice for the wrought wire clasp design.
Class III and IV RPD retainer clasp designs for tooth-supported RPDs include circumferential or Akers’ clasps and rotational path partials for exceeding esthetic expectations.
Minor Connectors
Minor connectors include all connecting links between the major connector or base of the RPD and all other units of the partial to include denture base retentive elements. Most minor connectors extend from the major connector to a prepared surface of the tooth. These prepared surfaces include various types of rests that provide vertical support for the RPD such as: occlusal, cingulum, ball, channel, and incisal rests. Occlusal rests are spoon shaped and are deepest at the center of the preparation while having a horizontal dimension of one-third the width of the occlusal table at the marginal ridge. Cingulum rests are ideally chevron shaped with the deepest point at the apex of the chevron and have a horizontal dimension of one-third the lingual surface of the tooth. Ball rests, also known as modified cingulum rests, are located mesial or distal to the natural cingulum. Channel rests extend from the marginal ridge to the long axis of an abutment tooth. They tend to direct forces down the long axis of a posterior abutment tooth. Channel rests are also commonly used on a distal abutment molar that has a mesial inclination for a rotation path of insertion RPD. Incisal rests are unesthetic, increase length of fulcrum, and interfere with occlusion in protrusive movements. Thus, incisal rests are highly undesirable if anterior esthetics are high on the expectation list.
Indirect Retainers
Properly designed indirect retention reduces ANP torsional leverage on the principal abutments. They assist in stabilizing the RPD against horizontal movement, splint the teeth they contact against movement, and act as auxiliary support for the major connector (Figure 13). An indirect retainer acts as a third point of reference for visual indication to determine the need to reline the RPD when it fails to fully seat as the extension base is displaced toward the edentulous ridge (Figure 17).
Summary
The keys to success with removable partial dentures are proper clinical assessment of the oral condition, diagnostic mounted study casts, determining desirable and undesirable undercuts, proper tooth modification, impeccable impressions, accurate master casts, copious clinical and technical communication on design, and occlusal harmony (Figure 18). As we go forward into this digital future of removable prosthetics, design options will be integrated into software based on variables present (Figures 19 and 20).
Technology with digital workflow processes will change removable prosthodontics as we currently know it, although human biology and biomechanics will not change. Technicians who accept these new digital tools will always be the masters of case design and manufacturing processes. Those who possess excellent knowledge in biology and bio-mechanic principles of RPD design plus digital solutions will have a true advantage in dental laboratories and prosthodontics of the future.
Acknowledgement
The author would like to thank European Chrome Dental Laboratory for providing images of their completed RPDs.
References
1. Jacobson T. RPD Design and Treatment Planning. Presented at Study Group; 1986.
2. Connelly M and Pagan W. Removable Partial Denture Theory and Design. Presented at Study Group; 2003.
3. Kennedy E. Partial Denture Construction. New York, NY: Dental Items of Interest Publishing Company; 1928.
4. Henderson D and Steffel V. McCracken’s Removable Partial Denture Construction. St. Louis, MO: C.V. Mosby Co.; 1969. design workflow process.
About the Author
Robert Kreyer, CDT
Prosthodontic Consultant
Cupertino, California