You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
Triggering at once the most gratifying, frustrating, and fearsome sentiments, dentistry in the visible section of the mouth is a complex undertaking, sometimes subtly but occasionally blatantly so. Cases involving implants disturb not only the dental architecture but also that of bone and gingiva, structures that change shape easily upon violation, further complicating matters. Despite strides in regenerative surgery and prosthetic manipulation, a natural-appearing relationship between papilla, surrounding mucosa, native teeth, and implant crowns is exasperatingly difficult to achieve. A functional, long-lasting anterior implant restoration is probable but one that is, moreover, indistinguishable from its indigenous neighbors is less feasible. Blame the extended epithelial connection between titanium alloy and mucosa, any inherent dearth of osseous or soft tissue and possibly capricious healing.1,2 Thus, the most pressing question is also the most superficial: how much tooth and gum does the patient expose upon smiling? To put things bluntly, what can the patient put up with (and his or her clinicians get away with) cosmetically? The combination of physical boundaries and patient tolerance determines the appropriate restorative solution for partial edentulism in the esthetic zone. The lip line is the primary determinant of esthetic success; a low lip line (exposure of less than 75% of teeth upon smiling) covers a multitude of sins.3 This notion is tempered by the fact that certain patients demand perfection regardless of whether anyone else sees their teeth. These patients possess a high esthetic concern and must be treated as if they had high smile lines. For them as well as those with average (exposure of 75% to 100% of teeth and only interproximal gingiva) and high (exposure of all teeth and a contiguous band of gingiva) smiles, treatment consists of possible augmentation of bone and/or mucosa, non-buccally-oriented implant placement, delivery and progressive alteration of interim restorations to refine tissue draping, and a precisely hued final prostheses. This article reviews treatment steps and decision points that the healthcare team and patient must undergo to reach a satisfactory, agreed-upon implant resolution to partial edentulism in the anterior area.
Patient-Doctor Harmony
Recognition of the limits of dentistry—the boundaries of current technology as well as those of the individual clinician and dental technician—is imperative. Total honesty with the patient and with oneself with respect to the predictability of care encourages trust, eases the treatment process, and, most importantly, preserves the patient–doctor relationship regardless of therapeutic particulars or even the eventual outcome. In the midst of persuading a patient to commit to treatment, it is all too tempting to overpromise results and gloss over the efforts required to accomplish them. There are, however, always temporal, psychological, and monetary costs to the patient, but the more thoroughly these are attended to or at least delineated in the beginning, the less the chance for untoward surprises, exasperation, and subsequent crumbling confidence during treatment.
The dentist must convey clearly to the patient that disturbances in the mucosal form, namely apically displaced margins and blunted or even absent papilla, may occur in spite of exceptional surgical and restorative efforts. The implant-retained crown may appear longer than its counterparts and the soft tissue thinner or off-color (ie, redder or darker) depending on the width of keratinization. Of course, due to limits of contemporary treatment or unreasonable, even nonsensical, client demands, not every patient desire may be mitigated completely. Both doctor and patient need to be realistic about expectations before initiation, during, and after completion of treatment, and it is imperative for a dentist not to oversell treatment or his or her abilities. If implant rehabilitation mandates multiple invasive procedures and long healing periods that still cannot guarantee predictable outcomes, especially if the situation involves a patient with some amount of body dysmorphia, then consider alternative therapy (ie, a tooth-borne fixed partial denture, resin-bonded fixed prosthesis, or removable partial denture). Case planning entails not only diagnosis and the logical plotting of clinical phases but also the psychological readying of the patient to comprehend treatment and accept its consequences, ideal or not. Without a simpatico understanding between all parties involved in care, treatment tempts at least dissatisfaction if not disaster.
Evaluation of Implant Spacing
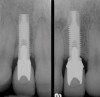
Adequate mesio-distal space is the first clinical criterion that must be met (Figure 1 through Figure 5). The basic tenet of the healthcare profession is “do no harm.” Therefore, if anticipated implant placement would infringe upon the periodontal support of bordering teeth, collide with tooth structure, or breach other vital anatomical formations (ie, nerve bundles), it must be expunged from the treatment plan or the plan modified to create enough leeway room. Indeed, the conservation and reformation of papilla depends on the presence of certain widths of interproximal bone, which sustain presence of the mucosa. The establishment of biological width and the presence of the microgap, or interface between the abutment and implant, at or below the crest of bone often gives rise to circumferential alveolar resorption around its head; as such, the surgeon must allow for enough latitude between a fixture and its closest neighbors to compensate for any osseous loss and maintain enough proximal bone to uphold the papilla.2,4 In fact, curtailing the influence of the microgap, an area prone to micro-movement and bacterial ingress, is a current subject of investigation. Platform switching, in which a wide implant platform is coupled to a narrower abutment, medializes the microgap and removes it from direct contact with bone, thus lessening crestal resorption.2 A recent meta-analysis suggests that a 0.4-mm or greater diameter mismatch between the platform and abutment enhances the potential for bone conservation, though the amount of crestal structure preserved compared to non-switched implant restorations is minimal (a difference of 0.37 mm), and there appears to be no difference in implant survival between switched and traditional platforms.5
Single implants, or those located between two natural teeth, typically require a minimum of 1.5 mm of bone between the edge of the implant and the root surface.4 In the case of replacement of a lone maxillary central incisor, there should be a distance at least 2 mm to 2.5 mm between tooth and fixture, as the peak of bone sandwiched between centrals is customarily wider. The space between an implant and another should be even farther apart; this scenario requires no less than 3 mm of interproximal bone. Two maxillary central incisor implants ought to be at least 4 mm to 4.5 mm apart to support the naturally wider configuration in this area. Taking into account the information above and considering the natural width and emergence profile of teeth, the standard implant diameter used for lateral incisors is less than 4 mm, while the diameter used to substitute central incisors and canines does not typically exceed 5 mm.6 Obviously, the recommended diameter varies depending on the individual patient’s dental idiosyncrasies. Some patients simply do not possess enough mesio-distal crestal bone or room between the roots for esthetic conventional implant placement. Replacement of a failing peg-sized maxillary lateral incisor, for example, may require orthodontic movement to create sufficient interdental space (Figure 6 through Figure 9). If the patient will not or cannot manage implant space creation, alternative therapies include restoration with a removable appliance, resin-bonded fixed prosthesis, or conventional fixed partial denture.
Evaluation of Bone
Bone sets the tone; in other words, implant function and soft tissue form hinge on the volume and quality of osseous material surrounding the fixture. An implant placement yields ideal esthetics only when it conforms to a prosthetically driven position; the orientation of the desired emergence profile equals the path of implant insertion. If this preferred path fails to fall within the bounds of the alveolus, then the requisite bone must be built by the surgeon to conform to the desired fixture direction. There are specific ridge dimensions required to support the implant initially and withstand future resorption from occlusal forces.7 Primary stability of an implant calls for at least 1 mm of buccal and of lingual bone. The prevention of facial recession, however, requires a minimum of 2 mm of buccal support.8 The necessary interproximal bone measurements vary depending on the existence of adjacent teeth or implants but do not fall below 1.5 mm (see “Step 4: Evaluation of Soft Tissue”). Inevitably, some level of alveolar turnover occurs after tooth extraction, with buccolingual resorption exceeding apicocoronal loss. Deficits after 4 months of healing average 3 mm to 6 mm horizontally and 1 mm to 2 mm vertically.9,10 Socket preservation, or the placement of bone grafts with or without membranes immediately into the extraction site, appears to diminish horizontal bone loss to 1 mm to 1.5 mm and maintain vertical height or even augment it by 1 mm.9,11,12 To be sure, instead of inserting graft material into the fresh socket, one could slip in an implant. Recent studies, including a Cochrane systematic review, refute the idea that immediate implantation eclipses conventional placement with respect to preserving bone, implant survival, or esthetic factors in the long-term, though there is data that it rates better esthetically in the short-term (less than 2 years after loading).13-15 Immediate implant insertion cuts treatment time length but is indicated only if there is a lack or removal of active infection, primary stability, a thick buccal plate, sufficient interproximal bone, optimal insertion angle, and patient understanding of possible complications.
For already-edentulous sites, appraisal of bone quantity entails radiographic analysis, including computed tomography (CT) scan imaging, and possible bone sounding (Figure 10 through Figure 14). Computed tomography is useful in every case but remarkably so when clear signs of resorption present. With a CT scan and related software, the dentist has the ability to envision the ridge form in all three dimensions, assess the location, amount and type of bone regeneration required, and virtually perform implantation, permitting detailed treatment scheduling and rendering surgery more precise. Meticulous ridge assessment clarifies if and when hard tissue grafting should occur. Any regenerative technique (eg, guided bone regeneration, onlay grafting, ridge splitting) used to rectify non-space–making defects, those that extend beyond the envelope of native bone, must be executed and the site left to mature fully before implant placement. This process may take 3 months to 1 year, with healing time directly proportional to volumetric expansion. Moderate to large space-making ridge deformities benefit from pre-implant grafting, especially if the clinician suspects any possibility that they would preclude primary stability of the fixture. In contrast, a small space-making defect, such as a dehiscence or fenestration, allows for bone augmentation (eg, guided bone regeneration, graft alone, osteotome-mediated expansion) at the time of implant placement (Figure 15 through Figure 20). Note that it is easier to remedy buccolingual defects than apicocoronal ones, but that definitive esthetics arguably relies more heavily on the abundance of vertical bone, which scaffolds the papilla. A patient with a large non-space–making vertical defect must expect compromised esthetics.
Evaluation of Soft Tissue
Ample alveolar housing and amenable bone quality ensure implant survival but do not promise its esthetic appeal, a condition reliant chiefly on the soft tissue morphology. The existence (or creation) of solid, wide bone physically buttresses the buccal free gingival margin (FGM) and papilla.8 Around maxillary anterior dentition, the standard distance between the facial FGM and alveolar crest is 3 mm, and the distance between the tip of the papilla and interproximal bone (ie, height of the papilla) hovers around 4.5 mm.16 Analogous measurements around a single implant ape those seen around teeth; interestingly the height of the implant–tooth papilla averages 3.85 mm.17 Nonetheless, the presence of adequate bone cannot guarantee that the mucosal form will follow natural contours. Even around normally erupted teeth, the soft tissue drape sometimes deviates from the osseous architecture, which typically follows the curve of the cementoenamel junction (CEJ), due to root proximity, adjacent tooth support, and tissue thickness.18 In the end, it is the patient’s congenital tissue biotype that governs how well an implant restoration will blend into its surroundings. There are two major tissue biotypes: thick/flat and thin/scalloped (Table 1).19
It is much easier to mask the presence of an implant in a patient with a thick/flat biotype for several reasons. Thick bone is less prone to resorption, encourages revascularization during healing, and bodily holds up the soft tissue. Similarly, thick gingiva recedes less, is easier to handle surgically, and heals faster due to its vascularity. Perhaps most significantly, there is simply less need for highly undulated tissue due to the inherently stunted papilla shape, apically located contact point, and compressed gingival contour. These naturally low esthetic demands benefit all parties.
On the other hand, mimicking a thin/scalloped biotype proves taxing to even the most experienced dental team, and more often than not, the dentist must forewarn the patient as early as possible about inconsistent cosmetic outcomes. Recall that the mean height of papilla adjacent to single implants is a bit less than 4 mm (3.85 mm).17 Accordingly, the prevalence of complete or nearly complete papilla fill (Jemt scores 2 and 3) around single implants is 100% when the distance between the contact point and crestal bone is less than 4 mm.17,20 Any increase in this distance dramatically reduces the chance of papillary fill; for example, if the contact point-to-bone space increases to 6 mm, there is only a 50% likelihood of full papilla. The projected papillary height between two implants is even shorter, closer to 3 mm (mean 3.4 mm).21 Thin tissue, especially if non-keratinized, provides another obstacle to ideal cosmetics because it tends to recede around restorations, becomes inflamed easily, and allows prosthetic margins to show through.22,23 Thus, a patient who has a thin/scalloped biotype with papilla frequently exceeding 4 mm in height may notice disparities in the soft-tissue drape (ie, black triangles, shortened papilla, longer teeth, and darkened or discolored marginal mucosa) around single and multiple implants compared to the existing dentition. The ability of the patient to accept these differences depends on the lip line and, needless to say, how fastidious about orofacial appearances he or she is. Increasing the width and volume of keratinized mucosa with an apically positioned flap, free gingival grafting, connective tissue grafting, or acellular dermal grafting prior, during, or after implantation, with earlier intervention being more favorable, improves general mucosal health and cosmetics at the buccal margin but cannot entirely convert a thin/scalloped biotype into a thick/flat one, especially in the critical interproximal regions.14,24 Even mucosal intervention begun as early as the time of tooth extraction, such as creation of a provisional with an ovate pontic extending 1 mm to 3 mm below the mucosal margin that aims to retain the gingival emergence profile of the original tooth, may not safeguard an intrinsically fragile tissue type.16,18,25 The treatment team must convince the patient to rein in his or her expectations, particularly if the plan includes multiple implants, and forfeit ideal soft tissue esthetics for high functionality or seek another restorative solution.
Implant Placement
Based on the tenets discussed above, implant placement should adhere to several morphologic guidelines, all of which center around the notion that the fixture must follow the path of the ideal emergence profile (ie, be prosthetically friendly) (Table 2). Use of a surgical guide aids the practitioner in this mission, but even with a guide, the clinician must at all times have a kinesthetic sense of where the implant needs to be. Insertion in the anterior zone favors palatal over buccal angulation because a platform tilted facially may thin the alveolar plate, thus promoting recession, and also result in a tooth that appears to protrude or be discolored due to abutment visibility through the crown or mucosa. Palatal orientation, with maintenance of at least 2 mm of buccal bone, offers the restorative dentist more flexibility with the emergence profile and resists tissue resorption.8,18 Similarly, the apicocoronal position of the implant at the buccal influences these factors. Natural teeth exhibit a free gingival margin-to-osseous crest distance of 3 mm at their mid-facial aspects, and this observation applies to adjacent implant restorations as well. To complement the facial gingival contour of its neighbors, the platform of the implant should lie roughly 3 mm apical to the desired mucosal margin of the crown, which should line up more or less with the free FGM of the existing anterior dentition.18,26,27 A platform located further apically but supracrestal or at the crest may cause a deep, hard-to-clean peri-implant pocket to form; one that lies subcrestal may initiate buccal bone loss and subsequent soft tissue recession in a patient with thin, non-augmented buccal bone. Even so, a more apically situated implant provides plenty of room for shaping an archetypal emergence profile; the same cannot be said of a more coronally located implant (< 3 mm from platform-to-mucosal margin), which stymies any normal-appearing emanation of the crown from the maxilla. Finally, the interproximal bone and its anticipated overlying papilla depend on the mesiodistal space between the implant platform and the adjacent tooth or implant; the wider the distance, the greater the odds of bone retention and papillary formation, though the papilla expected are more likely to be short and squat than long and thin.17,21
Considerations at Second-Stage Surgery, Implant Temporization, and Final Restoration
Placement of the healing abutment in a two-stage implant sequence offers another opportunity to scrutinize the tissue form and improve upon the mucosa, albeit only to a restricted degree. Multiple surgeries in the same site progressively diminish the body’s capacity to heal as fibrosis develops along with fewer patent vessels, and by the time second-stage uncovering comes, the ability for repair, let alone regeneration, fades somewhat. All the same, there are a number of methods to maintain, mold, and grow gingiva at the implant site. Papilla-sparing exposure of the implant head involves removing mucosa only over the cover screw using a scalpel or a tissue punch.28 Such means do not bulk up buccal or papillary volume and, therefore, should be limited to areas where ideal contours already exist. More commonly, some kind of additive approach is required, ranging from connective tissue grafting; guided soft tissue augmentation achieved by burying healing abutments below the flap, thus compelling tissue to granulate into the created vertical gap; and papilla regeneration, which fashions interproximal tissue by splitting, sectioning, and/or sliding the immediate surrounding tissue into the papillary space.29-34 Perhaps the simplest and most effective scheme to create facial bulk and increase keratinization is to orient the crestal incision palatally over the implant site, connecting lingual line angle to lingual line angle with the cut, elevate a full- or split-thickness buccal flap, secure the healing abutment, position the flap facial and slightly coronal to the abutments, and suture in place, letting secondary intention healing occur.
At this stage, anchoring of a well-constructed implant-level provisional to the implant, either in lieu of a healing abutment placement or shortly thereafter, further sculpts the tissue, defining a natural emergence profile, and priming the interproximal space for papilla.35 Contingent on the silhouette of the temporary, particularly the shape at the cervical base, the marginal mucosa pulls up or down. At the facial margin, an increase in the subgingival contour spurs apical migration of the FGM, whereas a flatter subgingival outline generates coronal displacement. A greater subgingival contour at the proximal aspect, conversely, squeezes the papilla tip coronally; a decreased contour there moves the papilla apically.36 An interim restoration that brings about ideal soft-tissue morphology, however, does not automatically fit in tooth shape-wise with the rest of the dentition.37 The dental team may need to sacrifice cosmetics in both ways. Ultimately, the extent to which the prosthodontist is able to alter the emergence profile and fabricate a beautifully draped permanent crown hangs on the amount of bone and mucosa the patient possesses. Severe ridge deficiency sometimes makes black triangles and masking with gingiva-colored ceramics inevitable, and the patient may need to accept implant function over form or seek a surrogate option.
Conclusion
A number of factors combine to make implant restoration functionally and esthetically viable in the maxillary anterior zone. From a biomechanical standpoint, the amount of bone present is the most imperative, and it follows that any bone preservation or augmentation should occur as early as possible. The soft tissue tends to conform to the osseous shape; if the alveolar structure is malformed or delicately wrought, the emergence profile of the implant too becomes imperfect or tough to replicate. Hence reproducing the profile of the natural periodontium in patients born with thin/scalloped biotypes around implant restorations is notoriously problematic. Converting the implant site to a thick/flat biotype produces a mismatch between the indigenous teeth and the artificial one, yet not attempting to augment or otherwise adjust the hard and soft tissue just about ensures cosmetic failure (ie, black triangles, receded facial mucosa, marginal discoloration) if not mechanical disintegration as well. Practically speaking, the easiest implant patient to care for is one with both a low lip line and a low concern for esthetic harmony, but the resourceful practitioner plans each treatment case with as much meticulousness, restraint, and aboveboard communication. Any initially straightforward-seeming case may take a turn for the worse if breaches of biological, surgical, restorative, or case managerial principles arise. Successful fulfillment of the following steps is crucial to a satisfying cosmetic result:
• Diagnosis
• Treatment sequencing
• Communication of diagnosis, sequencing, potential treatment consequences, and esthetic outcomes to patient
• Hard- and soft-tissue preservation and/or regeneration
• Prosthetically driven implant placement, with specific buccolingual, apicocoronal, and mesiodistal orientation
• Provisionalization to finalize tissue contours prior to final prosthetics
References
1. Cochran DL, Hermann JS, Schenk RK, et al. Biologic width around titanium implants. A histometric analysis of the implanto-gingival junction around unloaded and loaded nonsubmerged implants in the canine mandible. J Periodontol. 1997;68(2):186-198.
2. Hermann JS, Buser D, Schenk RK, et al. Biologic width around titanium implants. A physiologically formed and stable dimension over time. Clin Oral Implants Res. 2000;11(1):1-11.
3. Tjan AH, Miller GD, The JG. Some esthetic factors in a smile. J Prosthet Dent. 1984;51(1):24-28.
4. Tarnow DP, Magner AW, Fletcher P. The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J Periodontol. 1992;63(12):995-996.
5. Atieh MA, Ibrahim HM, Atieh AH. Platform switching for marginal bone preservation around dental implants: a systematic review and meta-analysis. J Periodontol. 2010;81(10):1350-1366.
6. Hebel KS, Gajjar RC. Cement-retained versus screw-retained implant restorations: achieving optimal occlusion and esthetics in implant dentistry. J Prosthet Dent. 1997;77(1):28-35.
7. Grunder U, Gracis S, Capelli M. Influence of the 3-D bone-to-implant relationship on esthetics. Int J Periodontics Restorative Dent. 2005;25(2):113-119.
8. Spray JR, Black CG, Morris HF, Ochi S. The influence of bone thickness on facial marginal bone response: stage 1 placement through stage 2 uncovering. Ann Periodontol. 2000;5(1):119-128.
9. Iasella JM, Greenwell H, Miller RL, et al. Ridge preservation with freeze-dried bone allograft and a collagen membrane compared to extraction alone for implant site development: a clinical and histologic study in humans. J Periodontol. 2003;74(7):990-999.
10. Schropp L, Kostopoulos L, Wenzel A. Bone healing following immediate versus delayed placement of titanium implants into extraction sockets: a prospective clinical study. Int J Oral Maxillofac Implants. 2003;18(2):189-199.
11. Lekovic V, Kenney EB, Weinlaender M, et al. A bone regenerative approach to alveolar ridge maintenance following tooth extraction. Report of 10 cases. J Periodontol. 1997;68(6):563-570.
12. Vance GS, Greenwell H, Miller RL, et al. Comparison of an allograft in an experimental putty carrier and a bovine-derived xenograft used in ridge preservation: a clinical and histologic study in humans. Int J Oral Maxillofac Implants. 2004;19(4):491-497.
13. Botticelli D, Berglundh T, Lindhe J. Hard-tissue
alterations following immediate implant placement in extraction sites. J Clin Periodontol. 2004;
31(10):820-828.
14. Esposito M, Grusovin MG, Polyzos IP, et al. Interventions for replacing missing teeth: dental implants in fresh extraction sockets (immediate, immediate-delayed and delayed implants). Cochrane Database Syst Rev 2010(9):CD005968.
15. Araujo MG, Sukekava F, Wennstrom JL, Lindhe J. Ridge alterations following implant placement in fresh extraction sockets: an experimental study in the dog. J Clin Periodontol. 2005;32(6):645-652.
16. Kan JY, Rungcharassaeng K, Kois JC. Removable ovate pontic for peri-implant architecture preservation during immediate implant placement. Pract Proced Aesthet Dent. 2001;13(9):711-715.
17. Choquet V, Hermans M, Adriaenssens P, et al. Clinical and radiographic evaluation of the papilla level adjacent to single-tooth dental implants. A retrospective study in the maxillary anterior region. J Periodontol. 2001;72(10):1364-1371.
18. Kois JC, Kan JY. Predictable peri-implant gingival aesthetics: surgical and prosthodontic rationales. Pract Proced Aesthet Dent. 2001;13(9):691-698.
19. Olsson M, Lindhe J. Periodontal characteristics in individuals with varying form of the upper central incisors. J Clin Periodontol. 1991;18(1):78-82.
20. Jemt T. Regeneration of gingival papillae after single-implant treatment. Int J Periodontics Restorative Dent. 1997;17(4):326-333.
21. Tarnow D, Elian N, Fletcher P, et al. Vertical distance from the crest of bone to the height of the interproximal papilla between adjacent implants. J Periodontol. 2003;74(12):1785-1788.
22. Bouri Jr A, Bissada N, Al-Zahrani MS, et al. Width of keratinized gingiva and the health status of the supporting tissues around dental implants. Int J Oral Maxillofac Implants. 2008;23(2):323-326.
23. Chung DM, Oh TJ, Shotwell JL, et al. Significance of keratinized mucosa in maintenance of dental implants with different surfaces. J Periodontol. 2006;77(8):1410-1420.
24. Cairo F, Pagliaro U, Nieri M. Soft tissue management at implant sites. J Clin Periodontol. 2008;35(8 Suppl):163-167.
25. Priest G. Developing optimal tissue profiles implant-level provisional restorations. Dent Today. 2005;24(11):96-100.
26. Davarpanah M, Martinez H, Celletti R, Tecucianu JF. Three-stage approach to aesthetic implant restoration: emergence profile concept. Pract Proced Aesthet Dent. 2001;13(9):761-767.
27. Saadoun AP, LeGall M, Touati B. Selection and
ideal tridimensional implant position for soft tissue aesthetics. Pract Periodontics Aesthet Dent. 1999;11(9):1063-1072.
28. Auty C, Siddiqui A. Punch technique for preservation of interdental papillae at nonsubmerged implant placement. Implant Dent. 1999;8(2):160-166.
29. Beagle JR. Surgical reconstruction of the interdental papilla: case report. Int J Periodontics Restorative Dent. 1992;12(2):145-151.
30. Matthews DP. The pediculated connective tissue graft: a novel approach for the “blown-out”’ site in the esthetic zone. Compend Contin Educ Dent. 2008;29(6):350-357.
31. Misch CE, Al-Shammari KF, Wang HL. Creation of interimplant papillae through a split-finger technique. Implant Dent. 2004;13(1):20-27.
32. Nemcovsky CE, Moses O, Artzi Z. Interproximal papillae reconstruction in maxillary implants. J Periodontol. 2000;71(2):308-314.
33. Salama H, Salama M, Garber D, Adar P. Developing optimal peri-implant papillae within the esthetic zone: guided soft tissue augmentation. J Esthet Dent. 1995;7(3):125-129.
34. Scharf DR, Tarnow DP. The effect of crestal versus mucobuccal incisions on the success rate of implant osseointegration. Int J Oral Maxillofac Implants. 1993;8(2):187-190.
35. Touati B, Guez G, Saadoun A. Aesthetic soft tissue integration and optimized emergence profile: provisionalization and customized impression coping. Pract Periodontics Aesthet Dent. 1999;11(3):305-316.
36. Touati B. The double guidance concept. Pract Periodontics Aesthet Dent. 1997;9(9):1089-1094.
37. Froum SJ, Cho SC, Francisco H, et al. Immediate implant placement and provisionalization—two case reports. Pract Proced Aesthet Dent. 2007;19(10):621-630.
About the Authors
Michael Sonick, DMD
Private Practice
Fairfield, Connecticut
Debby Hwang, DMD
Private Practice
Fairfield, Connecticut