You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
The treatment of mandibular edentulism using dental implants is now well established as a biologically sound treatment option. More than 40 years after Swedish orthopedic surgeon Per-Ingvar Brånemark introduced the process of transforming oral function in the edentulous patient using endosseous dental implants, a picture of success has emerged that is recognized worldwide. The use of one or two implants to retain a mandibular overdenture and the use of four or more implants to support and retain a fixed dental prosthesis is widely known to provide improved function and increased satisfaction in the edentulous patient when compared to conventional denture therapy.1-6
The contemporary literature demonstrates a high degree of survival over the 10- to 20-year time horizon when implants are placed in the parasymphyseal mandible and restored with an implant-retained overdenture (IRO) or with an implant-supported fixed prosthesis (ISFP).7-10 These studies invoke inclusion and exclusion criteria that favor success, benefit from the local factors of mandibular bone quality and quantity, and commonly employ the use of an opposing maxillary denture. However, all the studies indicate high and lasting rates of implant survival. Less well documented and perhaps equally significant is the quality of the prosthesis, its longevity and maintenance requirements, and the related issues of patient-perceived satisfaction. There is also a history of common limitations associated with dental implant therapy for the
edentulous mandible.
The commonly prescribed IRO and ISFP prostheses are based upon denture fabrication techniques that use methyl methacrylate “acrylic” resin chemistry and cross-linked denture teeth. These materials serve as the functional substrate and esthetic foundation of the implant-based prostheses for the edentulous mandible. Support for the acrylic-veneered prosthesis has commonly been provided by gold-based dental alloy frameworks and, more recently, computer numeric controlled (CNC)-milled titanium or chromium-cobalt frameworks. The functional stresses—impact and imposed bending—endured by the esthetic veneer must be supported by and transmitted through the framework and the components to the supporting implants. The data for IRO and ISFP prostheses suggests that the incidence of complications with these prosthetic components is greater than the failure of the implants11 (Figure 1 and Figure 2). The materials, designs, and techniques used in the production of implant-supported prostheses for the treatment of mandibular edentulism require further consideration.
One hypothesis to explain the prosthetic failures and complications associated with the IRO and ISFP is that the mechanical environment established by implant placement is inadequate to permit proper construction of a robust and resilient IRO or ISFP prosthesis. Three different factors are essential to defining this mechanical environment (Figure 3). One is the magnitude of forces—specifically, bending moments, which are dependent on the magnitude of the load and the length of any cantilever. The second is the resistance of the prosthesis (of a defined material) against these relatively high and repetitive loads. The third factor is the biology of bone and its innate ability to respond to loading environments.
The aim of this report is to provide simple rules for treatment planning dental implant therapy in the edentulous mandible that both acknowledge and control the mechanical environment. This ultimately influences the success of both the endosseous dental implants and the prosthesis, and can offer lasting success for treatment of mandibular edentulism.
In order to provide a conceptual framework to manage the treatment of mandibular edentulism using dental implants, the three aforementioned factors affecting implant and prosthesis longevity have been addressed and are embodied in three “rules” for treatment planning (Table 1). For any IRO or ISFP, there must be a minimum of 10 mm of alveolar dimension (inferior/superior) and a minimum of 10 mm of interocclusal (restorative) dimension measured from the soft-tissue ridge crest to the occlusal plane. Additionally, for an ISFP, the anterior/posterior distribution of implants (commonly referred to as A-P spread) must be greater than 10 mm. Together, these three rules are referred to as the “Rules of 10.” This report will provide the rationale to support these general rules and illustrate their application in the treatment of mandibular edentulism.
Rule No. 1
Inferior/Superior Dimension of the Mandible Must be ≥ 10 mm
This rule states that the minimum alveolar dimension sufficient to support an IRO or implant-supported fixed denture (ISFD) prosthesis must be equal to that required to use implants of approximately 10 mm in length.
The use of implants of 10 mm or less in length for ISFD is well defined and successful. More than a decade ago, Brånemark and co-workers12 compared the outcome of ISFD treatment using implants of greater than 10 mm and less than 10 mm after 10 years. The outcome with different lengths of 3.75-mm machined surface implants revealed no difference in implant survival after 10 years. In a more recent 5-year prospective evaluation, Gallucci and others13 confirmed a high (100%) implant survival rate associated with treatment of mandibular edentulism using ISFD supported with 4, 5, or 6 implants of between 8 mm and 16 mm. In all cases, implant failures occurred before loading. A recent evaluation of 119 patients rehabilitated with four implants to support mandibular ISFD revealed a 99.1% success rate.14 There is little information that indicates the use of longer implants improves the survival of implants placed in the parasymphyseal edentulous mandible. It has also been suggested that longer implants may be required to resist the function of long cantilever prostheses. There is little clinical data to support or refute this notion. A 3-dimensional (3-D) finite element model demonstrated that implant length had no appreciable effect on stress distribution at the bone/implant interfaces when loaded by a cantilever prosthesis, suggesting that implant length does not dictate survival.15
Some added concern is focused on the IRO. One evaluation revealed a 93.9% success rate for implants supporting an IRO, and the authors concluded that implant-retained overdentures are an established treatment modality, with implant success rates that are very similar to the results obtained with fixed-implant-supported prostheses.16 A long-term examination of a two-implant mandibular IRO specifically considered the impact of implant length as one variable affecting implant survival. A high survival rate (95.5%) was recorded after 20 years of loading. Although 21% of implants were 8.5 mm or shorter, implant length and bone quality did not affect implant survival.17 The conclusions that may be drawn are that implants of approximately 10 mm have equally high survival in the parasymphyseal mandible for both IRO and ISFD, and that increasing implant length beyond 10 mm does not improve biologic outcomes in the ISFP with an appropriately designed cantilever. Thus, a mandible of 10 mm height, or inferior-to-superior dimension, is sufficient for an IRO or ISFP.
Conventional concepts for planning implant therapy have focused on bone quality and quantity.18 However, when considering the parasymphyseal mandible, rarely is type III and type IV bone encountered. Further, ridge resorption frequently results in a tall mandible that displays narrow buccolingual dimension (< 5 mm) near the ridge crest (Figure 4). In such cases, the use of alveolectomy to move the ridge crest inferiorly enables creation of a wider platform for implant placement (> 5 mm) and ensures that the osseous crest is at least 10-mm to 12-mm inferior to the planned occlusal plane (Rule No. 2). Paradoxically, ISFD or IRO treatment is facilitated by marked alveolar resorption. Thus, more favorable prosthetic scenarios involve residual mandibles of 10 mm to 15 mm in height, while the more challenging prosthetic scenarios are associated with large residual alveolar ridges (eg, after extraction). Infrequently, mandibles of less than 10 mm superior-to-inferior dimension are encountered. When four implants of 10 mm cannot be placed in a severely resorbed mandible, additional implants of shorter dimension may be considered. For example, in an 8-mm mandible, the use of 8-mm or 9-mm implants might be considered if additional implants are included. Mandibular fracture is not common, but is recognized as a serious potential complication among high-risk individuals.19
Rule No. 2
Interocclusal (Restorative) Dimension Measured from Ridge Crest to Occlusal Plane Must be ≥ 10 mm
The interocclusal (restorative) dimension directly impacts the quality and integrity of both an IRO and an ISFP. Both overdentures and fixed prostheses require a minimal dimension to provide structural integrity and to permit the establishment of proper contours in support of comfort, mastication, and speech.
When planning for implant placement, it is essential to first understand the planned position of the prosthetic teeth. In other words, plan down from the occlusal plane and not up from the osseous crest. This assures better control of the restorative dimension. The location of the occlusal plane is defined by proper denture construction at the appropriate vertical dimension of occlusion. While it is beyond the scope of this discussion, widely accepted anthropomorphic averages suggest that the distance from the mandibular incisal edge to the reflection of the buccal vestibule is approximately 18 mm.20 Therefore, if an existing denture measures less than 15 mm to 16 mm from the incisal edge to the buccal flange, there may be cause to reconsider the vertical dimension of occlusion and/or the placement of the occlusal plane.
This concept of restorative dimension was initially addressed by Phillips and Wong21 and reiterated by Lee and Agar22; however, there is little data in support of this inferior-superior dimension for planning of a mandibular IRO or ISFP. Practically, the restorative dimension for any implant prosthesis includes four key components, each with its own minimum dimension. They are: 1) the transmucosal dimension (biologic width) of approximately 2 mm; 2) a supramucosal abutment height (0 mm to 2 mm) that permits hygiene; 3) a framework or attachment height between 3 mm and 5 mm; and 4) acrylic veneer thickness greater than 2 mm (Figure 5). It must also be acknowledged that the replacement mandibular teeth should accommodate their full contours. The average height of mandibular anterior teeth is approximately 10 mm.23 A minimum 10 mm of restorative space places average-size mandibular prosthetic teeth precisely at the soft-tissue crest with only a minimal dimension for the prosthetic components.
It becomes evident that the planning of an implant-supported or implant-retained prosthesis for the edentulous mandible begins with defining a superior-inferior reference, namely, the occlusal plane. Space accommodation for the dimension and location of teeth, frameworks, attachments, retaining abutments (balls, bars, etc), and biologic width will direct planning of implant position. Finally, the location of the osseous crest in relationship to the planned implant position dictates the extent of the alveolectomy required (Figure 6). Jensen and colleagues provide an excellent review of the surgical and prosthetic considerations for the proposed alveolectomy and describe it as the creation of a mandibular “shelf.” In addition to establishing restorative space and alveolar width, the shelf design facilitates visualization of the inferior alveolar nerve, inspection of any lingual concavities, and collection of bone stock for any secondary grafting.24
This approach differs from the evaluation of bone as a primary step in the planning of mandibular implant prostheses. This second rule is essential for providing a robust and lasting fixed or removable prosthesis supported or retained by dental implants.
Rule No. 3
Anterior/Posterior Distribution of Implants Must be at Least 10 mm for the ISFP
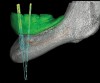
The ISFD was originally envisioned for treatment of mandibular edentulism by using the abundant bone of the mandibular parasymphysis. A cantilever design of the ISFD was inherent to the solution, using multiple anterior implants. The implants must be able to support functional loads at the posterior occlusal contacts via the cantilever. These loads, however, are magnified within the framework and components, and potentially at the implant/bone interface. In the early conceptualization of this therapy, the anterior-posterior distribution of dental implants was recognized as a key factor affecting the incidence of complications in the cantilevered mandibular ISFP. To counteract the imposed bending moments of the loaded cantilever, maximum distribution of implants was recommended. This anterior-posterior distribution of implants is referred to as the “A-P spread.” Clinicians were quick to point out that there were anatomic constraints for implant placement in the parasymphyseal mandible. Compared to curved or V-shaped mandibles, square-shaped mandibles often provide little anterior-posterior dimension anterior to the inferior alveolar nerve (Figure 7 through Figure 9). Additionally, anatomic variations in the inferior alveolar nerve (eg, anterior loop) are not uncommon25 and can reduce the available A-P spread.
A number of different models have been used to estimate the proper cantilever length in relationship to the A-P spread. These approaches include the use of photoelastic models, piezoelectric strain sensors, and finite element models. The results are diverse and the majority examined the stresses that accumulate at the implant bone interface. Interestingly, the focus on the implant, per se, does not match the clinical situation where implant failures are infrequent and prosthesis complications are more prevalent.
Any discussion of cantilever length requires that: 1) the position of the distal-most implant be anticipated; and 2) the number of teeth to be provided distal to that implant be defined. For the purposes of establishing a concept that meets the needs of most patients, the goal is to have the distal implant in the distal-most location that does not impose on the inferior alveolar nerve, which is generally located in the canine or first premolar region. Further, distal inclination of the posterior implants may place the prosthetic interface even more distal in the first premolar region.26
The all-on-four concept generally requires that posterior teeth beyond the first premolar are supported by a cantilever. Efforts to reduce or eliminate the cantilever by distal orientation of terminal implants are advocated. Bridge screws emerging at the first premolar or molar position can be achieved in this way. Malo has reported that this approach is associated with high implant and prosthesis survival over 10 years.26 In 2011, Malo reported on 245 patients in whom 980 implants were placed and immediately loaded. The cumulative patient-related and implant-related success rates were 94.8% and 98.1%, respectively, at 5 years and 93.8% and 94.9%, respectively, at 10 years.26
One other key factor contributing to the overloading of these components is prosthesis misfit. However, the accuracy of contemporary impression materials and the introduction of precision-milled frameworks for the ISFP reduce the prevalence of prosthetic misfit and its impact on the therapeutic outcome. The geometric distribution of the implant-abutment and the abutment-prosthesis interfaces remain the significant features of ISFP therapy that can be clinically managed to reduce complications.
When considering the number of teeth to be provided distal to the canine or first premolar site, the minimal provision of one additional premolar and one molar is sufficient to meet the esthetic and functional requirements of most individuals.27 These general guidelines can be converted to linear measurements. The average dimension of a mandibular premolar is approximately 6 mm, and that of the mandibular first molar is approximately 10 mm.23 Thus, a cantilever of 16 mm can suffice to provide function and esthetics. The functional relationship between the cantilever length and the A-P spread (Figure 7 through Figure 9) has been debated. More than 30 years of opinion, experimentation, and calculation have generated an array of suggested solutions. To provide the broadest range of success for the largest set of patients, a conservative estimate of this functional relationship should be selected. For a mandible with no more than four implants to be restored with a rigid framework, utilizing a cantilever length to A-P spread ratio of 1.5:1 has been advised.28 Thus, for the ideal situation of four implants placed in the parasymphyseal mandible with the distal-most implants located in the first premolar region, a cantilever of approximately 15 mm (one premolar and molar tooth) requires 10 mm of A-P spread. This represents the third Rule of 10.
Applying the Rules of 10
Several key steps are required for using the Rules of 10 in the treatment of mandibular edentulism. The previously mentioned reference points (ie, occlusal plane and osseous crest) must be firmly established. To assure accurate measurement, all treatment should begin with the proper fabrication of complete dentures and verification of ideal tooth position (Figure 10 and Figure 11).
Rule No. 1 requires a volumetric assessment of the edentulous mandible with cone-beam computed tomography (CBCT). However, other important information can be found in the radiographic process, and no radiograph should be made for ISFP treatment-planning purposes without the presence of a radiographic stent. The resultant image(s) should display the location of the planned prosthesis in relation to the mandible.
Rule No. 2 requires that the plane of occlusion is properly located and the appropriate vertical dimension of occlusion is defined. If the patient is also edentulous in the maxilla, this involves the fabrication of ideal maxillary and mandibular dentures. The dentures will define the location of the occlusal plane and mandibular tooth position, where the mandibular denture can be duplicated in radiopaque acrylic for a radiographic stent. The amount of alveolectomy needed can then be determined from the CBCT images.
Rule No. 3 requires an understanding of the anatomy of the edentulous mandible in relationship to the location of the planned prosthetic teeth, as well as the ability to translate this information to the implant placement, generally via a surgical guide. This can be accomplished practically in one of two ways. One method involves evaluation of the CBCT images using 3-D planning software (eg, Materialise Simplant®, Materialise Dental, www.materialise.com; NobelClinician™, Nobel Biocare, www.nobelbiocare.com) and then modifying a duplicate denture made from clear acrylic (Figure 10 and Figure 11). The other involves use of a third-party company to fabricate a digital surgical guide.
Conclusion
Dental implant therapy for the edentulous mandible has been successful. Data concerning implant survival is high and reflects the quality and quantity of bone available for osseointegrated implant function. The complications associated with both removable and fixed dental implant prostheses reflect the constraints of current materials and design limitations. The Rules of 10 assure that there is: 1) adequate bone for osseointegration and its long-term success; 2) sufficient dimension for fabrication of an esthetic, comfortable, and robust prosthesis; and 3) proper distribution of imposed forces from occlusal function within the prosthesis, at the implant/abutment screw interfaces, and at the implant/bone interfaces. Following these simple geometric and linear guidelines to treatment planning enables proper implant placement decisions that underscore robust and lasting prosthesis construction.
References
1. Raghoebar GM, Meijer HJ, Stegenga B, et al. Effectiveness of three treatment modalities for the edentulous mandible. A five-year randomized clinical trial. Clin Oral Implants Res. 2000;11(3):195-201.
2. de Grandmont P, Feine JS, Taché R, et al. Within-subject comparisons of implant-supported mandibular prostheses: psychometric evaluation. J Dent Res. 1994;73(5):1096-1104.
3. Fueki K, Kimoto K, Ogawa T, Garrett NR. Effect of implant-supported or retained dentures on masticatory performance: a systematic review. J Prosthet Dent. 2007;98(6):470-477.
4. Awad M, Locker D, Korner-Bitensky N, Feine J. Measuring the effect of intra-oral implant rehabilitation on health-related quality of life in a randomized controlled clinical trial. J Dent Res. 2000;79(9):1659-1663.
5. Emami E, Heydecke G, Rompré PH, et al. The impact of implant-support for mandibular dentures on satisfaction, oral and general health-related quality of life: a meta-analysis of randomized-controlled trials. Clin. Oral Implants Res. 2009;20(6):533-544.
6. Strassburger C, Kerschbaum T, Heydecke G. Influence of implant and conventional prostheses on satisfaction and quality of life: A literature review. Part 2: Qualitative analysis and evaluation of the studies. Int J Prosthodont. 2006;19(4):339-348.
7. Ekelund JA, Lindquist LW, Carlsson G, Jemt T. Implant treatment in the edentulous mandible: a prospective study on Brånemark system implants over more than 20 years. Int J Prosthodont. 2003;16(6):602-608.
8. Bryant SR, MacDonald-Jankowski D, Kim K. Does the type of implant prosthesis affect outcomes for the completely edentulous arch? Int J Oral Maxillofac Implants. 2007;22 Suppl:117-139.
9. Meijer HJ, Raghoebar GM, Batenburg RH, et al. Mandibular overdentures supported by two or four endosseous implants: a 10-year clinical trial. Clin Oral Implants Res. 2009;20(7):722-728.
10. Cooper LF Moriarty JD, Guckes AD, et al. Five-year prospective evaluation of mandibular overdentures retained by two microthreaded, TiOblast nonsplinted implants and retentive ball anchors. Int J Oral Maxillofac Implants. 2008;23(4):696-704.
11. Bozini T, Petridis H, Garefis K, Garefis P. A meta-analysis of prosthodontic complication rates of implant-supported fixed dental prostheses in edentulous patients after an observation period of at least 5 years. Int J Oral Maxillofac Implants. 2011;26(2):304-318.
12. Brånemark PI, Svensson B, van Steenberghe D. Ten-year survival rates of fixed prostheses on four or six implants ad modum Brånemark in full edentulism. Clin Oral Implants Res. 1995;6(4):227-231.
13. Gallucci GO, Doughtie CB, Hwang JW, et al. Five-year results of fixed implant-supported rehabilitations with distal cantilevers for the edentulous mandible. Clin Oral Implants Res. 2009;20(6):601-607.
14. Eliasson A. On the role of number of fixtures, surgical technique and timing of loading. Swed Dent J Suppl. 2008;(197):3-95.
15. Sertgöz A. Finite element analysis study of the effect of superstructure material on stress distribution in an implant-supported fixed prosthesis. Int J Prosthodont. 1997;10(1):19-27.
16. Ferrigno N, Laureti M, Fanali S, Grippaudo G. A long-term follow-up study of non-submerged ITI implants in the treatment of totally edentulous jaws. Part I: Ten-year life table analysis of a prospective multicenter study with 1286 implants. Clin Oral Implants Res. 2002;13(3):260-273.
17. Vercruyssen M, Marcelis K, Coucke W, et al. Long-term, retrospective evaluation (implant and patient-centred outcome) of the two-implants-supported overdenture in the mandible. Part 1: survival rate. Clin Oral Implants Res. 2010;21(4):357-365.
18. Lekholm U, Zarb GA. Patient selection and preparation. In: Brånemark PI, Zarb GA, Albrektsson T, eds. Tissue-Integrated Prostheses: Osseointegration in Clinical Dentistry. Chicago, IL: Quintessence Publishing. 1985:199-209.
19. Oh WS, Roumanas ED, Beumer J III. Mandibular fracture in conjunction with bicortical penetration, using wide-diameter endosseous dental implants. J Prosthodont. 2010;19(8):625-629.
20. Fayz F, Eslami A, Graser GN. Use of anterior teeth measurements in determining occlusal vertical dimension. J Prosthet Dent. 1987;58(3):317-322.
21. Phillips K, Wong KM. Vertical space requirement for the fixed-detachable, implant-supported prosthesis. Compend Contin Educ Dent. 2002;23(8):750-756.
22. Lee CK, Agar JR. Surgical and prosthetic planning for a two-implant-retained mandibular overdenture: a clinical report. J Prosthet Dent. 2006;95(2):102-105.
23. Scheid RC, Weiss G. Woelfel’s Dental Anatomy: Its Relevance to Dentistry. 8th Ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2011.
24. Jensen OT, Adams MW, Cottam JR, et al. The all on 4 shelf: mandible. J Oral Maxillofac Surg. 2011;69(1):175-181.
25. Greenstein G, Tarnow D. The mental foramen and nerve: clinical and anatomical factors related to dental implant placement: a literature review. J Periodontol. 2006;77(12):1933-1943.
26. Maló P, de Araújo Nobre M, Lopes A, et al. A longitudinal study of the survival of All-on-4 implants in the mandible with up to 10 years of follow-up. J Am Dent Assoc. 2011;142(3):310-320.
27. Kanno T, Carlsson GE. A review of the shortened dental arch concept focusing on the work by the Käyser/Nijmegen group. J Oral Rehabil. 2006;33(11):850-862.
28. Shackleton JL, Carr L, Slabbert JC, Becker PJ. Survival of fixed implant-supported prostheses related to cantilever lengths. J Prosthet Dent. 1994;71(1):23-26.
About the Authors
Lyndon F. Cooper, DDS, PhD
Stallings Distinguished
Professor and Chair
Department of Prosthodontics
University of North Carolina School of Dentistry
Chapel Hill, North Carolina
Bryan M. Limmer, DMD
Prosthodontics Resident
University of North Carolina School of Dentistry
Chapel Hill, North Carolina
W. Day Gates, DDS
Private Practice
Mobile, Alabama