You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
In the continuously shifting realm of digital dentistry, choices of imaging techniques can be of the utmost importance for precision in diagnosis, treatment planning, finalization, and tracking patient advancement. Notwithstanding the frequent emergence of novel technologies, careful consideration is necessary when navigating the plethora of available options. The gradual displacement of traditional dental impressions by intraoral scanning, coupled with the more recent integration of facial scanning as an adjunct to traditional 2D photography, has provided dental professionals with a reliable and enhanced method of capturing the oral anatomy and other structures related to the smile. For dental professionals who are committed to delivering superior full-arch implant-supported restorations, acquiring a comprehensive understanding of the capabilities and constraints of each imaging modality is essential. Moreover, clinicians and laboratory technicians should be prepared to address the challenges related to provisionalization as well as the prosthetic and surgical considerations associated with delivering full-arch implant prostheses using a fully digital protocol.
Intraoral Scanning
Although intraoral scanning offers clear advantages for many dental treatments,1 its implementation into full-arch implant procedures presents unique challenges,2 which result from various factors. At the heart of successful dental implant treatment lies the ability to accomplish precise planning and achieve accurate placement. Intraoral scanning holds the promise of high precision and accuracy-eliminating the need for conventional physical impressions while enhancing the overall efficiency of the treatment process.3 However, despite advancements in scanning technology, achieving consistent accuracy in full-arch implant cases remains problematic. To effectively tackle these challenges, innovative strategies have been developed that can help to reduce treatment times and enhance clinical outcomes.
The successful implementation of intraoral scanning for full-arch dental implant procedures hinges not only on state-of-the-art technology but also on specialized training and proficiency.4 Dental professionals must master the technical aspects of scanner operation and proper scanning techniques to ensure proper image acquisition. Navigating the technique-sensitive learning curve associated with intraoral scanning can be difficult, particularly for practitioners who are accustomed to traditional methods, but this education is essential because errors in scan acquisition and interpretation due to inadequate training or experience can compromise treatment outcomes.
The multitude of intraoral scanners available on the market adds complexity to implementation because each device possesses unique features, settings, and scanning protocols.5 Dental professionals should not need to invest in lengthy training programs and master intraoral scanning techniques solely to obtain what should be plug-and-play quality results; therefore, opting for a user-friendly scanner with a minimal learning curve is vital. This also reduces the risk of clinicians reverting back to traditional impression materials and effectively preventing the intraoral scanner from becoming anything more than a glorified paperweight. Furthermore, to aid practitioners and their teams, companies have developed intraoral scanning software with features powered by artificial intelligence, such as selective color removal, cross-arch stitching, and automatic occlusion techniques, which help overcome human challenges.
Related Challenges
Intraoral scanning for full-arch implant treatment often involves reaching anatomically challenging areas within the oral cavity, notably the posterior regions of the maxilla and mandible. Although intraoral scanners can offer convenience when compared with traditional impression materials, they do have limitations in hard-to-reach spots. The direct line of sight required for intraoral scanning can be obstructed by structures, such as the tongue, cheeks, or existing dental restorations. When certain areas prove challenging to scan effectively, it can lead to incomplete or distorted digital impressions. Moreover, the presence of metallic restorations and prosthetic components, such as implant abutments, can introduce artifacts that compromise scan quality, further complicating the precision of treatment planning and the optimization of restorations. To address these challenges, it is crucial to select ergonomically designed scanner heads and software that includes metal scanning options. In addition, employing various nonreflective or plastic soft-tissue retraction devices (eg, Scan Mate®, Armor Dental; Isolite®, Zyris; OptraGate®, Ivoclar) can enable clinicians to accurately scan their intended targets without reflecting the scanner light and creating errors (Figure 1).
Beyond hard-to-reach areas and the presence of metal, other factors, such as patient movement and the presence of saliva or blood can compromise the integrity of digital impressions, leading to inaccuracies with the placement and fit of the prosthesis. The dynamic nature of the mucosa (Figure 2) presents an additional layer of complexity because intraoral scanners may struggle to capture its anatomy with the same level of detail and accuracy as harder tissue structures, such as the teeth or keratinized tissue.6 The efficient management of soft tissue is crucial to the long-term success of implant therapy, impacting both the stability of restorations and the esthetic outcome. Failure to accurately capture detailed information about the soft tissue can compromise the success of implant restorations, potentially resulting in issues such as poor gingival health, peri-implantitis, and undesirable prosthetic emergence profiles.7 Ensuring proper bedding of keratinized tissue during the surgical phase can significantly enhance the success of intraoral scanning and implant-supported restorations. Furthermore, employing innovative drilling protocols and placing implants into adequate cancellous bone (Figure 3 and Figure 4) can alleviate strain on the overlying cortical bone, which typically exhibits less vascularity, and consequently, reduce alveolar remodeling, ultimately preventing bone loss around the crestal neck of the implant.
The challenges associated with intraoral scanning in full-arch dental implant procedures have profound clinical implications that extend beyond mere technical limitations. Inaccurate digital impressions can lead to misfitting implant restorations, which can result in complications such as soft-tissue inflammation, prosthesis fracture, bone loss, and implant failure (Figure 5 through Figure 7). The need for corrective procedures to address failures associated with inaccuracies can prolong treatment times as well as increase patients' discomfort and overall dissatisfaction. In addition, the financial implications of re-treatment cannot be overlooked because they may impose significant burdens on patients and practitioners alike. Inaccurate digital impressions may necessitate the fabrication of new restorations, additional surgical interventions, or modifications to the treatment plan-all of which can contribute to increased costs and treatment complexity as well as reduced patient satisfaction and confidence in the process. Patients who undergo full-arch dental implant procedures often have high expectations for the functional and esthetic outcomes of their restorations. Therefore, any discrepancies between the planned and actual results can lead to dissatisfaction and erode trust in the clinician's abilities.
Photogrammetry
Overcoming the obstacle of stitching together images with overlapping scan bodies and tissue has long impeded the accuracy of intraoral full-arch implant capture. However, a successful solution has been developed using dental photogrammetry systems (eg, iMetric iCam4D, Voxel Dental; PIC System, PIC Dental; MicronMapper, SIN 360). Photogrammetry involves attaching implant markers (ie, scan bodies, scan flags) to multi-unit abutments and then capturing multiple images from various angles using an extraoral optical scanner (Figure 8 through Figure 10).8 These images are then input into CAD software, matched to intraoral scans, and processed to create highly accurate virtual 3D models of arches and their surrounding structures. After inputting the data, technicians can seamlessly design tooth setups using a fully digital workflow.
Although photogrammetry devices are indeed effective, they can be quite costly, making it challenging for individual practices to afford them. This often leads to the need for shared ownership or borrowing arrangements between clinicians and laboratories, which can present logistical difficulties in real-world scenarios. However, as technology advances, the cost of photogrammetry units may decrease significantly, potentially increasing their feasibility for implementation in all dental practices. But at the present time, photogrammetry remains a low-utility modality for specialized procedures due to its affordability.
Fortunately, due to the cost of photogrammetry equipment, there has been a notable increase in the development of alternative accurate, yet cost-effective, methods of digitally capturing implant positions.
Splinted and Elongated Scan Bodies
Recognizing the limitations of intraoral scanning and aiming to mitigate its drawbacks, a novel approach has emerged involving the linking or bonding of scan bodies over multi-unit abutments (Figure 11).9 This innovative technique (eg, Optisplint®, Digital Arches; CAPS System, Dynamic Abutment Solutions; TRUSS Scanjig, DW Dental Solutions; Scan Ladder Direct, Scanladder; Tektonic, Asiga) successfully addresses the challenges associated with intraoral scanning for full-arch procedures, thereby enhancing the accuracy and efficiency of treatment. By physically linking the scan bodies, this approach enables either intraoral capture using a chairside method or, for enhanced precision, extraoral capture using a desktop scanner. The results have exceeded expectations, achieving a level of accuracy that is comparable to photogrammetry while also enabling the creation of a verification model. However, it's important to note some limitations, which include longer appointment times for acquisition when compared with photogrammetry and the inability to reuse the scan bodies due to their interconnected structure.
Another approach to tackle intraoral scan stitching issues using traditional multi-unit abutments involves using elongated scan bodies, some of which have unique individual shapes, to minimize the gaps between implants and permit continuous intraoral scanning without interruptions (eg, ArchBridge™, ROE Dental Laboratory; Nexus iOS, Keystone Dental Group; Scan Ladder Indirect, ScanLadder; Radar, PartMaker; EZ Ref, Evolve Dentistry) (Figure 12 and Figure 13). The use of distinct scan body shapes prevents the scanner acquisition software from duplicating, overlapping, or confusingly scanning the same object. These unique shapes facilitate simplified surface scanning of the scan bodies, which is particularly useful in immediate surgical cases where scanning is challenging due to a bloody field. Furthermore, importing uniquely shaped scan bodies into acquisition software programs with AI technology can enable scan body matching. After being captured, these scan bodies can be point-matched and aligned to the tissue scans in CAD software.
Regardless of which method is selected from the aforementioned options, a streamlined workflow can be implemented. However, a significant obstacle remains that prevents direct-to-final restorations: the restrictions posed by 2D-dimensional photography for approving or refining final restoration designs. This often discourages dental professionals, including laboratory technicians, designers, and clinicians, as well as patients from selecting a final restoration without intraoral try-ins.
Prosthetic Considerations
When developing treatment plans for patients, it is essential to conduct a thorough assessment to determine the most suitable final prosthetic solution. This assessment should carefully consider all of the relevant factors to ensure the most optimal outcomes. One crucial aspect to evaluate is whether a fixed or removable prosthesis is preferred by the patient. Fixed prostheses offer greater stability and functionality but may be associated with a greater financial and surgical burden. Alternatively, removable prostheses provide greater flexibility and ease of maintenance but may be less stable, which can affect the patient's confidence.
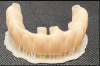
When a fixed prosthesis is desired, the decision regarding what type warrants careful consideration. The Misch system classifies fixed full-arch prostheses into three categories: FP1, FP2, and FP3.11 FP1 denotes a fixed prosthesis that replaces only the crown forms of missing teeth with no pink material to replace the gingiva. This type of prosthesis is indicated for edentulous arches that demonstrate minimal loss of hard and soft tissue (Figure 14). FP1 prostheses include bridges where artificial teeth are supported by natural teeth or implants. In contrast, FP2 prostheses replace the anatomical crown and root forms of missing teeth (Figure 15). These are intended to address edentulous arches with minimal to moderate loss of hard and soft tissue. And finally, FP3 protheses replace the anatomical crown and a portion of the soft tissue, incorporating pink material to restore the full complement of teeth and gingival tissues for arches that demonstrate a moderate to advanced loss of hard and soft tissue (Figure 16). Each option presents distinct benefits and considerations regarding function, esthetics, health, and long-term maintenance. By carefully assessing these factors, dental professionals can customize treatment plans to accommodate the individual needs and preferences of all patients. For example, addressing a smile that exhibits vertical maxillary excess may require extensive bone reduction to conceal the transition zone of an FP3 prosthesis, whereas an FP1 solution may require no or only minor bone removal, which may be more suitable for the patient and clinician.
Facial Scanning
Traditionally, assessing the appropriateness of an FP1 versus an FP2 or FP3 prosthesis for patients relied heavily on clinical evaluation and 2D photography. Despite the widespread use of 2D photography in dentistry, when compared with digital scanning, it presents limitations that can impede comprehensive diagnosis and treatment planning. Among these challenges is its flat representation of the face, which fails to capture crucial depth information that is essential to the accurate assessment of facial symmetry, proportions, and contours. In addition, because 2D photographs restrict clinicians to specific viewpoints, critical details that are vital to the understanding of 3D facial anatomy may potentially be overlooked. Other factors, such as distortion arising from camera angles, lighting, and lens characteristics, can further undermine the reliability of 2D images and complicate the interpretation of facial features and measurements. With 2D images, superimposing dental and facial structures accurately becomes a difficult task, and that can limit the accuracy of treatment planning as well as the clinician's ability to monitor treatment progress and outcomes.
Recent advancements have ushered in a more sophisticated approach to esthetic implant therapy. Clinicians and digital designers are now using cutting-edge hardware and software to integrate intraoral scans with 3D facial scans (Figure 17).12,13 This integration facilitates a comprehensive analysis of critical factors, such as lip position, smile design, and facial symmetry, and enables precise determinations of tooth size, length, width, and shape. The integration of 3D facial scans with intraoral scans transfers depth information about the face, providing clinicians with a comprehensive view of facial contours, volumes, and spatial relationships. This realistic depth visualization can improve the accuracy of diagnosis and treatment planning and, subsequently, aid in the selection of the most appropriate treatment.
Quantitative measurements (Figure 18) derived from 3D facial scanning software further enhance the precision of treatment planning, allowing clinicians to assess distances, angles, and volumetric changes with improved accuracy.14 These data points enable clinicians to make treatment decisions with greater confidence and help ensure optimal outcomes for patients. Facial reference measurements, including midline, width of the mouth, facial thirds, nasiolabial angles, interpupillary line, ala-tragus line, Frankfort horizontal plane, and more can be obtained from facial scans and interpreted in the office or forwarded to dental technicians for a more detailed analysis that can be electronically transferred, offering superior information when compared with 2D photographs.
Although the integration of 3D facial scans with intraoral scans has significantly advanced the overall process of evaluation, the incorporation of DICOM data from cone-beam computed tomography scans (Figure 19) has enabled practitioners to generate treatment plans that are even more detailed and precise. Such treatment plans are impossible to replicate using traditional 2D photography alone. By harnessing a combination of all available 3D scans in tandem and supporting the data with 2D photography, dental professionals can deliver highly effective personalized solutions, setting a new standard of care in prosthetic designs.
Surgical and Restorative Approaches
Once a full-arch treatment plan has been approved and a surgical plan has been created, clinicians face several decisions, including choosing either freehand surgery or guided surgery, an immediate loading protocol or delayed loading protocol for the implants, and provisional restorations that are prefabricated or fabricated after implant placement.15 Depending on whether or not multi-unit abutments will be used, additional decisions regarding fabricating coping or coping-free restorations and selecting the most appropriate screw system will need to be considered.
Stackable Surgical Guides
In the realm of digital treatment, excluding denture conversion, there are advantages and disadvantages to both prefabricated provisional restorations and provisional restorations fabricated after surgery. Prefabricated provisional restorations offer the benefit of immediate chairside availability, providing a stable same-day temporary solution. One approach to delivering a prefabricated provisional prosthesis involves using a stackable guided surgery solution (eg, CHROME™ GuidedSMILE, GuidedSMILE; CombiGuide™, ROE Dental Laboratory; Stackable Surgical Guide, All on Guide) (Figure 20 through Figure 23). This innovative approach employs a guide with a stackable design, whether metal or metal-free, to coordinate bone reduction, implant placement, and prosthetic delivery.16 Stackable surgical guides can simplify the final conversion protocol by utilizing a carrier guide over the foundational base that permits convenient luting of temporary cylinders to the appliance. Although this can be an excellent solution for immediate replacement, the prefabricated provisional prostheses require surgeons to position the implants within a narrow threshold. Another issue is that many patients in full-arch replacement cases are dentate. Complicated extractions in sites that are vital to the preplanned design can result in implants without sufficient primary stability for immediate loading and a delay in the delivery of the temporary prosthesis. Furthermore, severe adjustments in prefabricated provisional prostheses may render them unusable. Oftentimes, complicated cases are overengineered to compensate for surgical difficulties.
3D Printed Provisional Restorations
Given that guided surgery comprises only a small portion of the full-arch implant surgeries performed, there are also ongoing digital developments focused on immediate provisional solutions for freehand implant surgery. Historically, denture conversion and delayed loading were the only options; however, the emergence of in-office 3D printing has enabled clinicians to offer same-day or next-day provisional prostheses (Figure 24 and Figure 25).17 3D printing provides enhanced control over a provisional restoration's shape, color, and fit, and recent advancements in 3D printers and resin materials have significantly increased the strength of full-arch provisional restorations, reduced the time required to print them, and made coping-free solutions achievable in less than 15 minutes. When the implant position can be efficiently captured and the design time expedited, same-day 3D printed immediate provisional restorations may be the most desirable option. With 3D printing, clinicians can harness the benefits of digital dentistry to achieve improved functionality and esthetics by designing a provisional prosthesis that closely resembles the final restoration, eliminating the need for a prefabricated prosthesis or temporary cylinders. In addition, should the need arise, clinicians can choose alternate sites for implantation without compromising the provisional or overengineering the treatment plan.
When a postsurgical 3D printed provisional solution is chosen, it is crucial to capture the postsurgical implant position and relate it to the preoperative plan to expedite conversion and printing.18 In dentate cases, this process can be simplified by retaining a triad of scannable teeth (Figure 26), which enables the designer to quickly match the pre- and postsurgical positions. Alternatively, when a triad of scannable teeth is unavailable or in fully edentulous cases, preoperatively placing temporary anchorage devices in sites not planned for implantation, scanning them, and then rescanning them postsurgically can enable designers to match the pre- and postsurgical scans and utilize the preplanned arch design and occlusion.19
Metal-Free Prostheses
With advancements in metal-free designs, including improvements in strength and durability, metal-free prostheses made from materials such as zirconia or high-strength ceramics have become increasingly available (Figure 27). By eliminating titanium bases or copings from full-arch prostheses, patients benefit from restorations that are more biocompatible, and the need for excessive bone reduction can be minimized or eliminated. The delivery of an all-ceramic metal-free prosthesis that sits directly on multi-unit abutments is accomplished by using an appropriate prosthetic screw system (eg, Vortex™, Louisiana Dental Implant Lab; Powerball™, Xcell Dental Implant Process; Rosen Screw®, Rosen Implant Solutions; NobelProcera®, Nobel Biocare; Dess 19.018™, Dess; PRH 30™, S.I.N. 360). When compared with traditional multi-unit abutment screws, prosthetic screws specifically designed to affix prostheses without titanium bases or copings can offer versatility regarding the use of angulated screw channels and vertical positioning, and the shape of their heads provides greater surface contact and allows for greater material thickness along the screw's lateral walls, which reduces the potential for fracture and improves the overall esthetics (Figure 28 and Figure 29).
Conclusion
Although both intraoral scanning and facial scanning technologies hold immense promise for revolutionizing dental implant treatment, their application in full-arch implant procedures presents a myriad of challenges. Challenges involving accuracy, soft-tissue capture, limited access and visibility, and technical proficiency should be carefully considered and addressed to ensure successful treatment outcomes. Dental professionals should prioritize comprehensive training and ongoing education in order to be able to overcome these challenges and deliver optimal results for patients undergoing full-arch implant therapy. Furthermore, collaboration between clinicians, technicians, researchers, and technology manufacturers is essential to drive innovation and advancements in dental scanning technology, which will ultimately enhance its efficacy and reliability in complex implant cases. By understanding and navigating the complexities of scanning, dental professionals can unlock the full potential of digital dentistry and deliver safer, more predictable, and more esthetically pleasing full-arch implant-supported prostheses to their patients.
About the Authors
Isaac Tawil, DDS, MS
Founder and Co-director
Advanced Implant Education
Private Practice
Brooklyn, New York
Daniel Domingue, DDS
Private Practice
Lafayette, Louisiana
References
1. Lee SJ, Betensky RA, Gianneschi GE, Gallucci GO. Accuracy of digital versus implant impressions. Clin Oral Implants Res. 2015;26(6):715-719.
2. Alkadi L. A comprehensive review of factors that influence the accuracy of intraoral scanners. Diagnostics (Basel). 2023;13(21):3291.
3. Mangano FG, Hauschild U, Veronesi G, et al. Trueness and precision of 5 intraoral scanners in the impressions of single and multiple implants: a comparative in vitro study. BMC Oral Health. 2019;19:101.
4. Revell G, Simon B, Mennito A, et al. Evaluation of complete-arch implant scanning with 5 different intraoral scanners in terms of trueness and operator experience. J Prosthet Dent. 2022;128(4):632-638.
5. Di Fiore A, Meneghello R, Graiff L, et al. Full-arch digital scanning systems performances for implant-supported fixed dental prostheses: a comparative study of 8 intraoral scanners. J Prosthodont Res. 2019;63(4):396-403.
6. Nedelcu R, Olsson P, Thulin M, et al. In vivo trueness and precision of full-arch implant scans using intraoral scanners with three different acquisition protocols. J Dent. 2023;128:104308.
7. Tawil I. Avoiding peri-implantitis: key factors for improved clinical outcomes. Oral Health website. https://www.oralhealthgroup.com/features/avoiding-peri-implantitis-key-factors-improved-clinical-outcomes/. Published December 2, 2016. Accessed April 4, 2024.
8. Sánchez-Monescillo A, Sánchez-Turrión A, Vellon- Domarco E, et al. Photogrammetry impression technique: a case history report. Int J Prosthodont. 2016;29(1):71-73.
9. Tawil ID, Ganz SD. Fully digital full-arch? Continued advancements in full-arch implant restorations. Dent Today. 2023;42(4):50-57.
10. Ganz SD, Tawil I. Full-arch implant surgical and restorative considerations: innovative digital workflow using a verification jig with teeth. Dent Today. 2020;39(1):70-76.
11. Misch CE. Dental Implant Prosthetics. 1st ed. Mosby; 2004.
12. Hou X, Xu X, Zhao M, et al. An overview of three-dimensional imaging devices in dentistry. J Esthet Restor Dent. 2022;34(8):1179-1196.
13. Pozzi A, Arcuri L, Moy PK. The smiling scan technique: facially driven guided surgery and prosthetics. J Prosthodont Res. 2018;62(4):514-517.
14. Mai HN, Win TT, Tong MS, et al. Three-dimensional morphometric analysis of facial units in virtual smiling facial images with different smile expressions. J Adv Prosthodont. 2023;15(1):1-10.
15. Ganz SD, Tawil I. Full-arch implant surgical and restorative considerations: utilizing a full template guidance technique. Dent Today. 2019;38(9):72-78.
16. Ganz SD, Tawil I. Continued innovation for full-arch immediate loading: small access hole technology. Dent Today. 2021;40(4):64-69.
17. Ferguson R. Simplifying full-arch treatment with in-house 3D-printed surgical guides and immediate fixed provisional prostheses using only CBCT data. Compend Contin Educ Dent. 2020;41(10):521-526; quiz 527.
18. Lepidi L, Galli M, Grammatica A, et al. Indirect digital workflow for virtual cross-mounting of fixed implant-supported prostheses to create a 3D virtual patient. J Prosthodont. 2021;30(2):177-182.
19. Papaspyridakos P, Chen YW, Gonzalez-Gusmao I, Att W. Complete digital workflow in prosthesis prototype fabrication for complete-arch implant rehabilitation: a technique. J Prosthet Dent. 2019;122(3):189-192.